Removal of an intraosseous hemangioma of the frontal bone through an anterior hairline incision: a case report
Article information
Abstract
An intraosseous hemangioma of the frontal bone is typically removed via a coronal incision. This procedure, while effective, can be lengthy and may result in complications such as a prominent scar and hair loss. An alternative approach involves a direct incision in the forehead, which leaves a less noticeable scar and allows a quicker recovery. However, in this specific case, the patient declined both coronal surgery and surgery through a direct forehead incision due to cosmetic concerns. Therefore, we proposed an anterior hairline incision. A 35-year-old woman presented with a firm, non-mobile, palpable mass on her right forehead. Preoperative non-contrast computed tomography revealed a heterogeneous osteolytic lesion. We performed an excisional biopsy through the anterior hairline. Postoperative non-contrast computed tomography was conducted 2 and 6 months after surgery. The wound was clean and free of complications, and there was no local recurrence. Partial resection can reduce scarring for patients who are concerned about cosmetic outcomes. However, the potential for recurrence remains a significant concern. We present this case of an anterior hairline incision for a hemangioma located in the forehead, evaluated using serial computed tomography for both preoperative and postoperative imaging.
INTRODUCTION
Intraosseous hemangiomas are rare, benign, slow-growing tumors of the blood vessels, accounting for 0.7% of all bone neoplasms [1]. These tumors are most commonly found in the vertebral column and are seldom seen in the calvarium [2]. Given the rarity of facial bone hemangiomas, the majority of the existing literature comprises case reports, and there is a lack of consensus regarding the best management approach [3]. Traditionally, intraosseous hemangiomas in the frontal bone are removed via a coronal incision, a procedure that can be lengthy. The coronal approach can lead to complications such as a long scar and hair loss. Removal through a direct forehead incision has also been documented. Given the benefits of a smaller scar and quicker recovery time, this method could be a more favorable option compared to the coronal incision. However, in the case at hand, the patient declined both coronal surgery and surgery with a direct forehead incision due to cosmetic concerns. Therefore, we suggested an anterior hairline incision, approximately 3 cm in size, which would result in a scar, albeit a more acceptable one. Both the patient and the surgeons were satisfied with the clinical outcome of a barely visible scar following the removal of the intraosseous hemangioma via a small anterior hairline incision. In this report, we share our clinical experience with the removal of a frontal bone hemangioma through an anterior hairline incision, which yielded satisfactory cosmetic results.
CASE REPORT
A 35-year-old woman presented with a firm, immovable, and palpable mass on her right forehead, measuring 1.1 × 0.7 cm2 (Fig. 1). Other than this, her medical history was unremarkable. She had no other noticeable symptoms, except for the cosmetic issue caused by the mass. A preoperative non-contrast computed tomography (CT) scan revealed a heterogeneous osteolytic lesion, indicative of an intraosseous hemangioma (Fig. 1). We suggested removing the hemangioma through a coronal or direct forehead incision, which are the standard procedures. However, she declined these options due to concerns about potential cosmetic damage. As a result, we decided to make a small 3-cm transverse incision on the anterior hairline. We performed surgical tumor resection under general anesthesia, accessing the area through the patient’s anterior hairline. The dissection plane was established on the subperiosteal layer, and the soft tissue mass was almost entirely removed using curved mosquito forceps. The area of dissection measured approximately 2 cm in width by 3 cm in height. After confirming near-total soft tissue removal via endoscopy, we opted not to perform a superficial osteotomy due to the small size of the mass and potential for bleeding. To prevent hematoma, we inserted a Penrose drain and applied mild compressive dressings with elastic bandages. We surmised that the mass was likely benign based on its macroscopic appearance (Fig. 2). Partial resection was recommended, in line with a previously reported treatment algorithm for facial bone hemangiomas, as no other symptoms or signs were present [3]. Despite the risk of recurrence, the patient declined both the bicoronal incision and a direct incision on the forehead. We observed no intraoperative or postoperative bleeding. In this particular case, there was no communication with the frontal sinus, so no sealing of the frontal sinus was necessary. The wound was sutured layer by layer using 4-0 absorbable suture material and 4-0 nylon. The patient’s postoperative course was uneventful, and her appearance had significantly improved by the 6-month follow-up. We found no evidence of tumor recurrence (Fig. 3).
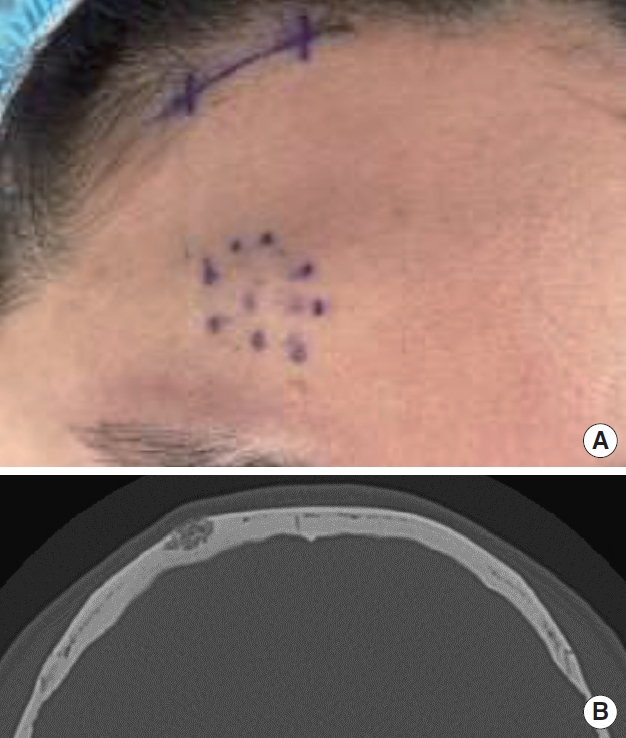
A 35-year-old woman presented with a firm, immovable, and palpable mass on her right forehead. (A) Preoperative photograph. (B) Computed tomography (CT) scan without contrast. Axial CT scan showing a well-defined lesion containing prominent trabeculae. The inner table is intact, but the outer table is displaced and has irregularly scalloped margins. No sclerotic margins are evident. The hemangioma penetrated the outer table, and the mass of the forehead protruded.

Histologic images (hematoxylin and eosin stain, ×400). A histological examination revealed an intraosseous hemangioma of the frontal bone, and histopathological evaluation revealed a tiny tissue fragment with proliferation of thin-walled, small vessels without endothelial nuclear atypia on the dead bone background, which is compatible with a hemangioma.
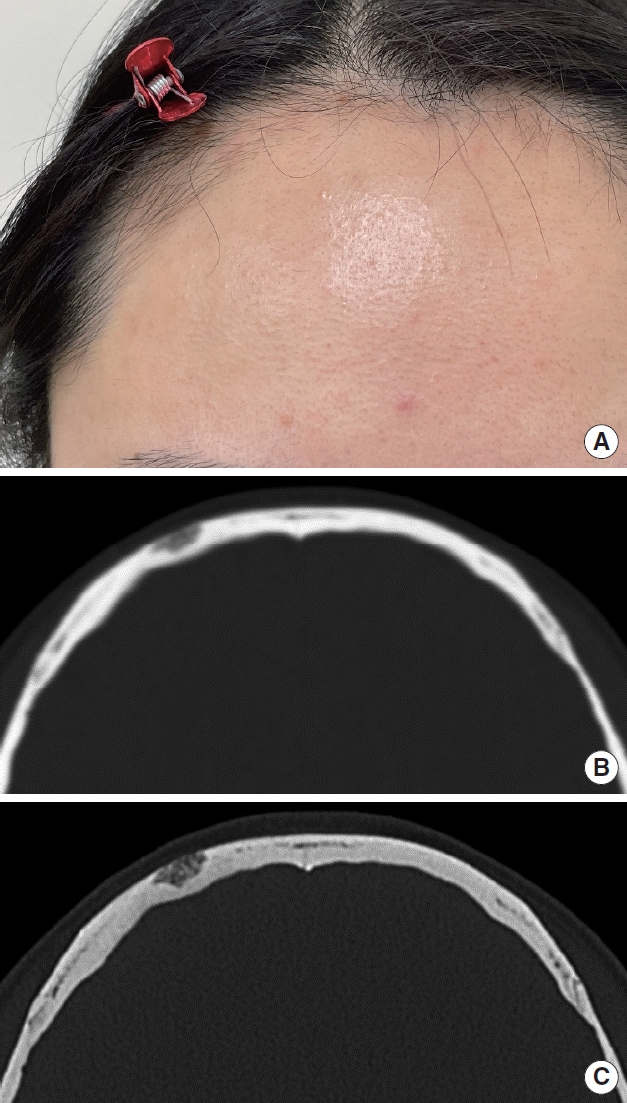
Postoperative images. (A) Six-month postoperative photograph. (B) Two-month postoperative computed tomography (CT) scan. Axial CT scan showing a well-defined lesion containing prominent trabeculae. The protruding part of the hemangioma was removed, and the rest remained. (C) Six-month postoperative CT scan. The results of surgery were maintained, and no additional changes in the lesion were observed at 6 months postoperatively.
DISCUSSION
Intraosseous hemangiomas are rare, benign tumors of vascular origin that typically arise in the vertebral body. Their occurrence in the skull is extremely rare, with only a handful of cases reported globally.
On November 10, 2022, we searched PubMed using terms including “intraosseous hemangioma AND anterior hair line incision” and “intraosseous hemangioma AND hair line incision,” and no reports were retrieved.
In the literature published as of 2022, 31 articles assessed the clinical course with intraosseous hemangioma using CT. Three of these studies [4-7] reported that CT was conducted on the first and twentieth postoperative days. Excluding one case that received only radiation therapy, 76 tumor cases underwent surgical intervention, with the extent of resection varying [7,8]. The case that received radiation therapy was initially misdiagnosed as breast cancer with skull metastasis. Out of the 76 patients, 60 had their tumors removed through craniectomy or en bloc resection via craniotomy, nine underwent subtotal resection, and two only had a biopsy without any surgical intervention [8,9].
CT is typically the first diagnostic tool used when an intraosseous hemangioma of the forehead is suspected. Given the benign nature of this condition, it is often recommended that clinicians simply monitor the hemangioma periodically if no symptoms are present [10]. Treatment is typically indicated in cases of mass effect, hemorrhage, or aesthetic concerns [3].
The primary goals of treatment are the complete surgical removal of the lesion and the preservation of a margin of healthy bone. While these lesions usually affect the outer table more than the inner table, achieving complete tumor removal at the diploe level can be challenging. A full-thickness resection of the calvarial or facial bone is often necessary to ensure a clear margin, which subsequently leaves a bony defect that necessitates reconstruction.
Although radical excision is frequently recommended, some patients with facial bone hemangiomas have been successfully treated with partial resection. Most individuals with these hemangiomas require surgery to correct a contour deformity. However, complete tumor resection typically involves a long incision and immediate reconstruction with bone grafts or alloplastic implants. In contrast, partial tumor resection not only necessitates a shorter surgical incision but also reduces blood loss, operation time, and potential reconstruction complications. In one study [3], the recurrence rate following subtotal resection was two out of five at a 7-month follow-up. In contrast, another study reported a recurrence rate of 0 out of nine [7].
The surgical excision of an intraosseous hemangioma in the frontal bone can be accomplished through a bicoronal approach, direct incision, or an anterior hairline incision. In this particular case, an anterior hairline incision was chosen for aesthetic purposes, resulting in a less noticeable scar and quicker recovery time. However, there are currently no established criteria for selecting an incision method, and further research is warranted.
Notes
Conflict of interest
No potential conflict of interest relevant to this article was reported.
Funding
None.
Ethical approval
This study was approved by the Dong-A University Hospital Institutional Review Board (IRB No. DAUHIRB-22-254).
Patient consent
The patient provided written informed consent for the publication and use of her images.
Author contributions
Conceptualization: Myung-Good Kim, Dong Min Lee. Project administration: Dong Min Lee, Tae-Seo Park. Visualization: Ji-An Choi. Writing - original draft: Myung-Good Kim, Jeong-Ho Ryu. Writing - review & editing: Jeong-Ho Ryu. Investigation: Myung-Good Kim, Jeong-Ho Ryu, Ji-An Choi. Resources: Dong Min Lee, Song-Hee Han. Supervision: Dong Min Lee, Tae-Seo Park, Ji-An Choi, Keun-Cheol Lee.
Abbreviations
CT
computed tomography
