Standardized surgical strategy for the treatment of preauricular sinus to reduce recurrence
Article information
Abstract
Background
Preauricular sinus (PAS) is a common congenital anomaly, and complete excision is recommended to prevent recurrence. However, PAS has a high recurrence rate as a result of incomplete removal due to the high variability of the sinus ramifications, making its treatment challenging. In this study, we standardized the surgical procedure to reduce the complications and recurrence rate and compared the postoperative results between the non-standardized and the standardized groups.
Methods
This retrospective study included 97 patients (120 ears) who had undergone PAS excision by a single surgeon between October 2014 and September 2022 and underwent at least 6 months of follow-up. After October 2018, all patients were treated using the standardized method, which comprised the use of magnifying glasses, exploration with a lacrimal probe, the use of methylene blue staining, and excision of a piece of surrounding normal tissue and related cartilage in continuity with the specimen. There were 38 patients (45 ears) in the non-standardized group and 59 patients (75 ears) in the standardized group.
Results
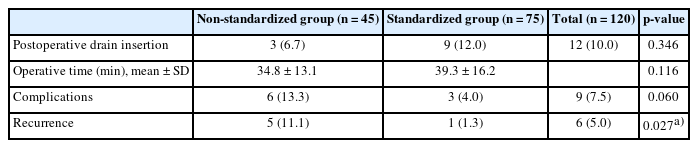
Recurrence was observed in six of 120 ears, indicating an overall recurrence rate of 5.0%. Recurrence occurred in five ears (11.1%) in the non-standardized group and one ear (1.3%) in the standardized group. The standardized group had a significantly lower recurrence rate (p= 0.027) than the non-standardized group.
Conclusion
We defined a standardized sinectomy protocol and used it for the surgical treatment of PAS. With this standardized method, we were able to reduce the rates of complications and recurrence without the use of a long incision.
INTRODUCTION
Preauricular sinus (PAS) is a congenital malformation of the preauricular area that was first described in 1864 [1]. It is caused by incomplete or defective fusion of the six auditory hillocks during preauricular development. PAS can be sporadic or inherited, and it has been mapped to a specific chromosomal location [2,3]. The incidence of PAS has been reported to be 0.1% to 10%, with a higher incidence observed in Asians and Africans than in Caucasians [3-5]. The most common location of the PAS opening is the anterior margin of the ascending limb of the helix, followed by the eminence of the cymba conchae; furthermore, these openings are more commonly seen in unilateral than in bilateral sinuses [3,6]. Only approximately 25% of patients with PAS experience symptoms [7]. Treatment is required for cases involving inflammation or infection with intermittent or chronic discharge [7,8].
Various surgical methods for the treatment of PAS have been published since the initial report of simple sinectomy in 1864; however, these can be broadly divided into the classic simple sinectomy approach and the supra-auricular approach (SAA). Simple sinectomy is associated with a relatively high recurrence rate (range, 0%–42%) because complete excision is difficult [9]. The SAA is associated with a lower recurrence rate (range, 0%– 23%) than simple sinectomy, but it is associated with problems such as dead space and long scars because extensive incision and dissection are required [9-11]. Several modifications have been proposed to reduce the recurrence rate associated with simple sinectomy, including the lacrimal probe, methylene blue staining, and magnification using a loupe or microscope. However, most studies have been retrospective case studies with a small sample size; therefore, there is a lack of substantial research on how these modifications affect outcomes. To reduce postoperative recurrence and complications and to achieve consistent PAS treatment results, we defined a standardized method of sinectomy, compared postoperative outcomes before and after standardization of this method, and analyzed the effects of standardization.
METHODS
Patients and standardization
The participants were patients who had undergone PAS excision by a single surgeon at our plastic surgery department between October 2014 and September 2022 and were available for at least 6 months of follow-up. Preoperative and postoperative demographic and clinical data from the patients’ medical records were retrospectively reviewed.
Surgery was performed in patients presenting with symptoms such as repeated discharge and swelling and in non-symptomatic patients when they requested for surgery. Antibiotics were administered to patients with preoperative inflammation or infection. Incision and drainage were performed for patients with an abscess. In such cases, surgery was performed 2 to 3 months after the incision and drainage and only after the infection had been controlled.
Sinectomy was used to perform PAS excision. The standardized method comprised all of the following: the use of magnifying glasses; exploration with a lacrimal probe; the use of methylene blue staining; and excision of a piece of surrounding normal tissue and related cartilage in continuity with the specimen. Only those who received all four procedures were enrolled in the standardized group, and those missing any of the four procedures were included in the non-standardized group. After October 2018, all patients were treated using the standardized method.
Surgical technique
The operator used magnifying glasses. During exploration via the insertion of a lacrimal probe in the opening of the PAS, the direction and depth of the sinus were identified and its margins were marked (Fig. 1A). An elliptical excision long enough to cover the full extent of the sinus, including the opening, was designed. In cases with a connection between the preoperative incision and drainage site and the sinus tract, a wider or a separate excision was made to excise the incision and drainage scar simultaneously (Fig. 1B). Next, methylene blue was instilled through a 22-gauge angiocatheter to stain the branches of the sinus tract (Fig. 1C). A sufficient amount of 1% lidocaine with 1:100,000 epinephrine was infiltrated to the incision and dissection site. After creating a skin incision, sharp Metzenbaum scissors and electrocautery were used to dissect the sinus away from the surrounding tissue (Fig. 1D). En bloc excision was performed, including a small amount of normal soft tissue (Fig. 1E); when the sinus was very close to the cartilage, some cartilage was also removed. Extra care was taken to avoid damage to the sinus wall in areas where methylene blue staining was observed. If the sinus wall was damaged, then povidone-iodine irrigation was additionally performed. After hemostasis, absorbable sutures were used to suture the surrounding cartilage and temporal fascia to reduce the dead space (Fig. 1F). The subcutaneous tissue and skin were then sutured layer-by-layer. A Penrose drain was inserted if necessary, and a compression dressing was applied. Antibiotics were administered for 5 days postoperatively. Recurrence was defined as symptoms, including discharge, inflammation, or infection. Postoperative complications, including seroma, hematoma, and infection, were also monitored.
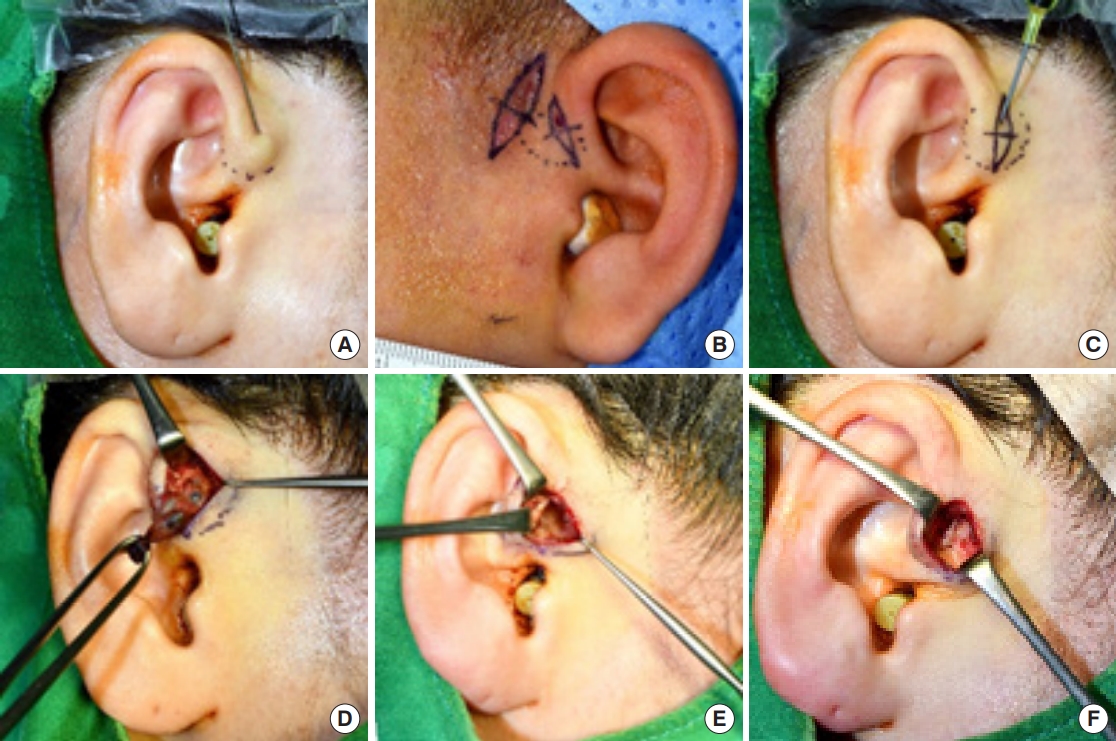
Standardized surgical procedure. (A) The depth and extent of the sinus are checked using a lacrimal probe and marked. (B) An elliptical skin incision is designed around the opening to include all of the sinus. In this particular case, an extra excision is designed because of the existence of a connection between the sinus and the incision and drainage scar. (C) A 22-gauge angiocatheter is inserted into the sinus opening and methylene blue is used to stain the sinus. (D) The inside of the sinus tract is stained with methylene blue dye to differentiate the sinus margin from the surrounding normal tissue. Sharp Metzenbaum scissors are used to carefully dissect the sinus from the surrounding tissue while avoiding damage to the fistula wall. (E) A small amount of normal tissue is included in the dissection to ensure complete excision of the preauricular sinus. (F) The cartilage and temporal fascia are sutured to reduce dead space.
Statistical analysis
SPSS 29.0 (IBM Corp.) was used for all statistical analyses. Patients who underwent bilateral surgery were considered as two separate cases. In comparison between the two groups, the significance of continuous variable differences (age and mean operative time) were compared with the independent t-test, and the categorical type variables were tested using the chi-square test. Although significant in the chi-square test, if more than 20% of cells have an expected frequency of less than 5, the Fisher exact test was performed. p<0.05 was considered statistically significant.
RESULTS
A total of 97 patients (120 ears; 42 male [43.3%]; 55 female [56.7%]), ranging from 13 months to 69 years of age (mean age, 27.0 years), were included. The PAS locations were the right side for 33 patients (34.0%), left for 41 (42.3%), and bilateral for 23 (23.7%). While 38 patients (39.2%) underwent the non-standardized procedure, 59 (60.8%) underwent the standardized procedure. Postoperative follow-up ranged from 6 to 101.3 months (mean follow-up, 41.9 months).
There were no statistically significant differences between the standardized and non-standardized groups in terms of age, sex, or PAS location. Seventeen patients (44.8%) in the non-standardized group and 22 (37.3%) in the standardized group experienced preoperative infection; this difference was not statistically significant (p=0.250) (Table 1). Two patients with uncontrolled infection underwent surgery because the infections did not respond to antibiotic treatment; both these patients were in the standardized group. The mean operative times were 34.8±13.1 minutes and 39.3±16.2 minutes in the non-standardized and standardized groups, respectively (p=0.116).
Of the 120 ears that were operated on, nine ears (7.5%) exhibited postoperative complications, such as seroma, hematoma, or infection. Specifically, complications were observed in six (13.3%) and three (4.0%) ears in the non-standardized and standardized groups, respectively (Figs. 2, 3); this difference was not statistically significant (p=0.060). Recurrence was observed in six of the 120 ears, indicating an overall recurrence rate of 5.0%. Specifically, recurrence was observed in five (11.1%) and one (1.3%) ears in the non-standardized and standardized groups, respectively, indicating that the recurrence rate was significantly lower after standardization (p=0.027) (Table 2). Of the patients who experienced recurrence, four patients improved with only antibiotics and incision and drainage and two patients experienced no further recurrence after revision surgery.

A 9-year-old boy with postoperative complications and recurrence after non-standardized sinectomy. (A) Preauricular sinus (PAS) with abscess formation on the left ear helical root. (B) Intraoperative view after complete excision of the PAS and incision and drainage scar. (C) Immediate postoperative view of the excised sinus and granulation tissue. (D) Postoperative view at 10 weeks showing intermittent discharge through a tiny opening at the operative site.

A 36-year-old woman without postoperative complications or recurrence after standardized sinectomy. (A) Preoperative image at 5 months after incision and drainage. (B) The preauricular sinus is completely excised, including some of the adjacent cartilage. (C) Immediate postoperative view of the excised specimen (note: some normal tissue is included in the specimen). (D) Image of a short, unnoticeable scar at 16 months postoperatively.
DISCUSSION
Although it is difficult to ascertain the precise number of patients with PAS that have undergone surgery in Korea, data from the South Korean Health Insurance Review and Assessment Service indicated that surgery was performed in 4,127 PAS cases in 2021; this is a relatively common procedure. However, a standardized surgical procedure for PAS has not been presented and very diverse techniques have been used till date.
The traditional technique is simple sinectomy. During this procedure, an elliptical incision is created around the sinus opening, the sinus tract is inspected with the naked eye, and the sinus is dissected and excised. However, PAS often forms a complex branching tract within the preauricular soft tissue; furthermore, in cases with previous inflammation or abscesses, the formation of fibrotic tissue can make it difficult to differentiate the sinus branches [12,13]. According to Kim et al. [14], a stratified squamous epithelium lumen, which is indicative of residual sinus tissue, was discovered in 73.7% of patients who underwent revision surgery for recurrent PAS. Therefore, complete excision, including all branches of the PAS, is important to minimize postoperative recurrence. However, with simple sinectomy, there is always a risk of incomplete excision, which results in a high recurrence rate.
The SAA, which was first introduced by Prasad et al. [15] in 1990, involves en bloc resection of the subcutaneous tissue and sinus between the temporalis fascia and helix and uses a much longer incision than simple sinectomy. This technique increases the simplicity of complete excision of the sinus without the need to follow the sinus tract and branches, which is required during simple sinectomy, resulting in a lower recurrence rate. However, the SAA leaves a long scar because the incision extends to the supra-auricular and/or postauricular area, and it is associated with the risk of seroma, hematoma, and depression caused by dead space [10,11,16]. A systematic review published in 2016 reported that the average recurrence rate of simple sinectomy was 5.5% (range, 0%–42%), whereas that of SAA was 2.2% (range, 0%–23%) [9]. Another systematic review reported recurrence rates of 8.1% for sinectomy and 1.3% for SAA; therefore, lower recurrence rates were observed with SAA according to both reviews [17].
Various modifications to reduce the recurrence rate associated with simple sinectomy have been suggested, including the use of a lacrimal probe, methylene blue staining, and magnification using a loupe or microscope. One study involving the use of a lacrimal probe and methylene blue staining compared the use of neither modification, the use of one of the two modifications, and the use of both modifications and found that using both modifications reduced the recurrence rate from 22% (using neither modification) to 0% [18]. Using a probe and methylene blue instillation reduced the recurrence rate compared to the use of methylene blue alone [19]. One study that used magnification, a lacrimal probe, and methylene blue instillation found a recurrence rate of 2.3% [20]. However, to the best of our knowledge, there have been no studies that have compared the effects of using each of these three modifications individually.
Recently, the importance of systematic and comprehensive quality assurance has been emphasized in medical research to achieve a certain level of treatment outcomes. Therefore, it is crucial to provide standards for surgical treatment and reveal the important factors responsible for discrepancies in treatment outcomes [21,22]. In this study, we analyzed the various existing surgical methods of treating PAS and then standardized the entire surgical procedure. We used a modified simple sinectomy technique and defined the standardized procedure as follows: the operator wore magnifying glasses, used a lacrimal probe to explore the sinus, used methylene blue instillation to dye the sinus tract, and included some of the surrounding normal tissue in the excision to ensure complete removal of the sinus. All procedures were performed by a single surgeon (HY), and we found that this standardization significantly reduced the recurrence rate (non-standardized: 5/45 cases, 11.1%; standardized: 1/75 cases, 1.3%; p=0.027). Moreover, after standardization, even though the rate of preoperative infection was relatively high (37.3%), the recurrence rate at 1.3% was much lower than the average recurrence rate of 5.5% reported for sinectomy by a previous systematic review, and it was even lower than the average recurrence rate of 2.2% reported for the SAA. In this study, recurrence was significantly reduced through standardization of the surgical technique using four specific modifications.
Since the ear is prominently visible and surgical procedures can result in ear deformities and excessive scarring, surgical treatments for the ear focus on minimizing both visible scarring and the risk of ear deformities [23,24]. Regarding postoperative scarring or deformity, our modified sinectomy used an incision length of approximately 1 to 1.5 cm, which was limited to the length of the sinus. This incision length is much shorter than that used during the SAA and the incision could be aligned with natural skin folds, resulting in only minimal scarring or deformity. Therefore, most scars were unnoticeable in our cases. In this study, no preoperative evaluation of the internal structure of the PAS was attempted. It may be beneficial for the reduction of recurrence by utilizing ultrasoundgraphy or fistulography before surgery to assess the internal structure of PAS and plan the surgery accordingly based on its complexity. Therefore, it is worth considering the inclusion of preoperative imaging evaluation in the standardization process.
However, this study had some limitations. An objective evaluation of the scarring or deformity was not performed. In addition, this was a retrospective study with relatively few cases. Although we limited the study to patients who underwent at least 6 months of follow-up, long-term monitoring is necessary to identify further recurrence. Finally, because the standardized procedure was only performed at a later time period, we could not exclude the possibility of reduced recurrence being attributable to improvement in the skill of the operator.
We defined and used a standardized sinectomy using magnifying glasses, a lacrimal probe, methylene blue staining, and the inclusion of a small amount of normal tissue in the excision of PAS. With this modified method, we were able to reduce the rates of complications and recurrence without the use of a long incision.
Notes
Conflict of interest
No potential conflict of interest relevant to this article was reported.
Funding
None.
Ethical approval
The study was approved by the Institutional Review Board of Daegu Fatima Hospital (IRB No. 2023-02-004) and performed in accordance with the principles of the Declaration of Helsinki.
Patient consent
The patients provided written informed consent for the publication and the use of their images.
Author contributions
Conceptualization: Hyeonjung Yeo. Data curation: Hannara Park, Jaemin Seong, Hyeonjung Yeo. Formal analysis: Hyochun Park, Hyeonjung Yeo. Methodology: Jaemin Seong, Hyeonjung Yeo. Project administration: Hyeonjung Yeo. Visualization: Hannara Park. Writing - original draft: Jaemin Seong, Hyeonjung Yeo. Writing - review & editing: Hannara Park, Jaemin Seong, Hyochun Park, Hyeonjung Yeo.
Abbreviations
PAS
preauricular sinus
SAA
supra-auricular approach