Concurrent presentation of porocarcinoma and basal cell carcinoma arising on a capillary malformation: a case report
Article information
Abstract
Porocarcinoma (PC) and basal cell carcinoma (BCC) are distinct skin cancers. Few studies have documented the occurrence of two concurrent types of skin cancers, and to the best of our knowledge, this represents the inaugural report of such a coexisting lesion arising from a capillary malformation. Herein, we report a case of concurrent PC and BCC presenting with capillary malformation. A 93-year-old woman visited our hospital with a protruding mass in her right nasal ala that appeared as a capillary malformation. A biopsy was performed on the skin lesion, and BCC was diagnosed. A wide excision was performed. Permanent biopsy revealed that the skin lesion was a PC with basal cells and squamous differentiation. The safety margin of the deep tissue margin was < 0.1 cm; however, considering the advanced age of the patient, further excision was deemed to not possess any benefits. This case illustrates the importance of recognizing the possibility of multiple skin cancers, even in patients with benign lesions such as capillary malformations. The rarity of this presentation highlights the importance of thorough investigation and histopathological examination of skin lesions in guiding appropriate surgical excision.
INTRODUCTION
The occurrence of concurrent skin cancer has been documented in several studies. When two distinct neoplasms are located adjacent to the same cutaneous site, the phenomenon is commonly referred to as a collision tumor [1,2]. Basal cell carcinoma (BCC), which arises from the basal cells in the epidermis, is the most common form of skin cancer. Various malignant skin tumors have been reported to co-occur with BCC at one site [3]. The occurrence of BCC and other skin cancers has been attributed to shared risk factors [1]. However, whether this is a coincidence or if there is a correlation between the two cancer types remains unclear. Although cases of concurrent occurrence of both skin cancer types have been reported, such instances are rare. Further research is required to better understand the relationship between BCC and other skin cancer types.
Porocarcinoma (PC) is a rare type of skin cancer that typically arises from sweat glands. To the best of our knowledge, its cooccurrence with BCC has not been previously reported [4]. In our patient, we observed both PC and BCC lesions in capillary malformations. Although certain studies have reported BCC de-velopment in vascular lesions, different skin cancer types occurring in capillary malformation have never been reported [5-7].
Herein, we present a rare case of concurrent PC and BCC originating from capillary malformation and emphasize the importance of accurate histopathological diagnosis.
CASE REPORT
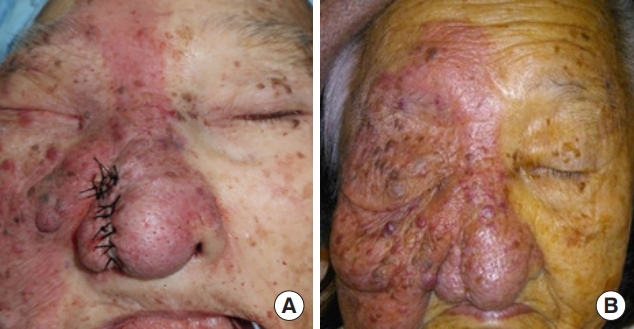
A 93-year-old woman presented at our hospital with a protruding mass in her right nasal ala. Although she had no underlying diseases, such as diabetes or hypertension, she had a capillary malformation on the right half of her face (Fig. 1). The protruding mass appeared on the capillary malformation, and apart from a partial excision performed 15 years previously, no other treatment history existed for the capillary malformation. The patient requested removal of the lesion because of its tendency to bleed. Preoperative biopsy confirmed a diagnosis of BCC, prompting the planning of wide excision and reconstruction.

A 93-year-old woman with a hemangioma on the right hemiface showing a protruding mass on the right nasal ala.
Before surgery, magnetic resonance imaging (MRI) was performed to confirm the extent of the lesion. The MRI confirmed a 3.4 cm exophytic mass with a depth of 2 mm, diagnosing it as BCC (Fig. 2). To assess the possibility of metastasis, chest computed tomography (CT), neck CT, neck ultrasonography, and wholebody positron emission tomography were conducted; however, no lymph node metastasis or distant metastasis was found.
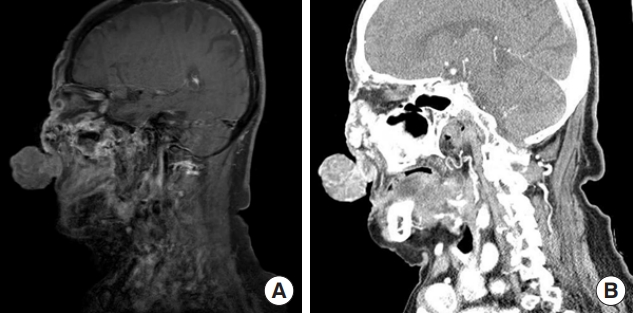
Preoperative images showing a 3.4 cm exophytic mass with a depth of 2 mm. (A) Magnetic resonance imaging and (B) computed tomography.
Wide excision and reconstructive surgery under general anesthesia were planned. The wide excision was performed with a 5 mm resection margin, and six samples were obtained, including the 12 o’clock, 3 o’clock, 6 o’clock, and 9 o’clock directions, as well as two deep margin samples for frozen section analysis, which confirmed no evidence of tumor involvement. The area was reconstructed using an advancement flap after subcutaneous dissection in both the lateral and medial directions. The patient was discharged on the 2nd postoperative day, and the wound healed well without any complications (Fig. 3). The permanent biopsy revealed that the skin lesion was a PC with basal cell and squamous differentiation, which had invaded the reticular dermis to a depth of 3 mm (Fig. 4). The diagnosis was classified as pT3NX according to the AJCC on Cancer Staging Manual, 8th edition criteria. Although the safety margin of deep margin tissue was <0.1 cm, considering the advanced age of the patient, further wide excision was deemed to have no benefits and the patient agreed to observation.
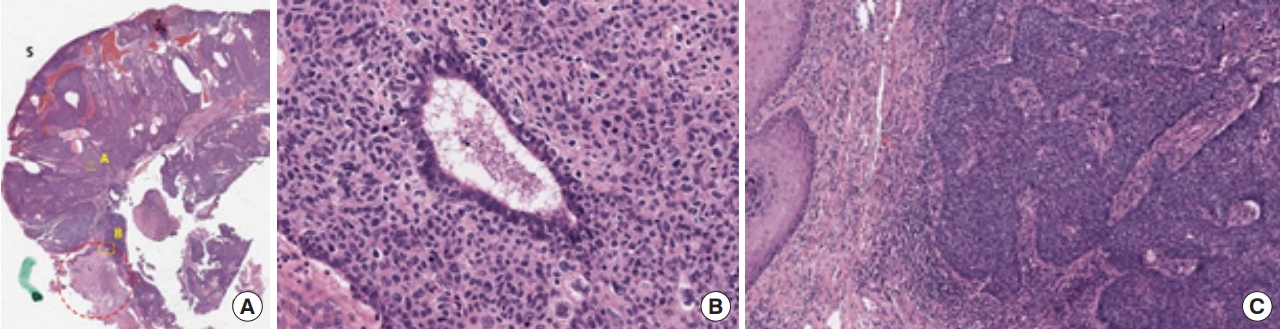
Tissue specimen stained with hematoxylin and eosin. (A) The area labeled “S” in the figure represents the superficial part of the tissue specimen, whereas the area labeled “D” represents the deeper part. Normal skin tissue can be observed (red dotted circle), and basal cell carcinoma (BCC) invasion is visible. Porocarcinoma has grown beyond the normal skin. Tissue specimen slide, magnified by ×12. (B) Photograph of area “A,” magnified by ×800, which shows the presence of a porocarcinoma. Misshapen nuclei and irregularly sized cells were observed, and ductal differentiation was visible. Clear fluid can be seen inside the duct, which is a characteristic feature of porocarcinomas originating from eccrine sweat glands. (C) Photograph of area “B,” magnified at ×400, which shows the invasion of normal skin by BCC. BCC forms nests, and the cells stand in a palisade pattern at the edge.
DISCUSSION
Herein, we present a rare case of PC and BCC occurring concurrently in a patient with a capillary malformation. BCC is the most prevalent type of skin cancer and has often been documented to co-occur with other skin tumors, such as collision tumors [2]. The occurrence of concurrent benign tumors, such as compound nevi and fibrous and vascular tumors, has been frequently reported [3]. Furthermore, documented cases of their co-occurrence exist with not only relatively common squamous cell and melanoma carcinomas but even rarer cancers, such as Merkel cell, sebaceous, and verrucous carcinomas [3,8].
PC is a rare skin cancer that arises from the intraepidermal part of the sweat gland [4], and its etiology is not well understood; however some cases are known to develop within a preexisting benign poroma [9]. PC commonly presents as a firm nodule or plaque of violet or erythematous color [10]. Although a standard treatment method for this rare cancer has not yet been established, wide excision is currently considered the mainstay of treatment and is often complemented by adjuvant chemotherapy or radiation therapy [10,11].
In this case, the patient presented with a mass that had been progressively growing over the course of 1 year, and exhibited a bleeding tendency of a protruding mass that is occasionally observed in PC patients. To the best of our knowledge, there exist no previous reports of PC occurring concurrently with BCC. What makes this case unique is that two different types of skin cancers were found in a long-standing capillary malformation. Several cases of BCC originating from various types of hemangiomas or vascular malformations have also been reported. In a report by Beer et al. [5], a case of BCC arising from a longstanding hemangioma was documented, whereas Feinmesser et al. [6] reported three cases of BCC arising from arteriovenous malformations [5-7]. Certain studies have suggested that the chronic inflammatory response that occurs in hemangiomas or vascular malformation lesions could contribute to the development of skin tumors. Skin cancers, including BCC, squamous cell carcinoma, and malignant melanoma, which develop in scars or chronic wounds, are commonly referred to as scar tissue carcinomas [12]. Similar to that in scar tissue carcinoma, a chronic inflammatory response can also occur. Epithelial or stromal changes can arise as a consequence of an initial skin tumor, potentially leading to the induction of another skin tumor [13].
Additionally, collision tumors can be triggered by factors including severe sun damage, multiple sunburn occurrences, and localized immunosuppression [14]. Therefore, ascertaining the medical history of the patient is crucial when encountering cases of collision tumors, as these factors can play a pivotal role in their development. However, the relationship between PC, BCC, and capillary malformations remains uncertain, and further research is needed to elucidate this potential association. In recent years, a collision tumor, defined as the coexistence of two or more distinct neoplasms within the same lesion, has been actively studied with numerous reports [15-19]. The occurrence of both BCC and PC in this case may provide clues for further investigation of collision tumors.
This case demonstrates the importance of recognizing the possibility of multiple skin cancers, even in patients with a history of long-standing benign lesions, such as capillary malformations. Consequently, being vigilant of skin lesions occurring on long-standing hemangiomas or vascular malformations and performing a diagnostic biopsy when malignancy is suspected is crucial. Furthermore, the rarity of this coexistent presentation emphasizes the need for a thorough histopathological examination of skin lesions to determine the appropriate surgical treatment.
Notes
Conflict of interest
No potential conflict of interest relevant to this article was reported.
Funding
None.
Ethical approval
The report was approved by the Institutional Review Board of Seoul National University Bundang Hospital (IRB No. B-2107/579-110).
Patient consent
The patient provided written informed consent for the publication and use of her images.
Author contributions
Conceptualization: Jong-Ho Kim. Data curation: Sunkyu Park. Writing - original draft: Sunkyu Park. Writing - review & editing: Jong-Ho Kim. Supervision: Jong-Ho Kim.
Abbreviations
BCC
basal cell carcinoma
CT
computed tomography
MRI
magnetic resonance imaging
PC
porocarcinoma