Orbital floor defect caused by invasive aspergillosis: a case report and literature review
Article information
Abstract
Fungal sinusitis is relatively rare, but it has become more common in recent years. When fungal sinusitis invades the orbit, it can cause proptosis, chemosis, ophthalmoplegia, retroorbital pain, and vision impairment. We present a case of an extensive orbital floor defect due to invasive fungal sinusitis. A 62-year-old man with hypertension and a history of lung adenocarcinoma, presented with right-side facial pain and swelling. On admission, the serum glucose level was 347 mg/dL, and hemoglobin A1c was 11.4%. A computed tomography scan and a Waters’ view X-ray showed right maxillary sinusitis with an orbital floor defect. On hospital day 3, functional endoscopic sinus surgery was performed by the otorhinolaryngology team, and an aspergilloma in necrotic inflammatory exudate obtained during exploration. On hospital day 7, orbital floor reconstruction with a Medpor Titan surgical implant was done. In principle, the management of invasive sino-orbital fungal infection often begins with surgical debridement and local irrigation with an antifungal agent. Exceptionally, in this case, debridement and immediate orbital floor reconstruction were performed to prevent enophthalmos caused by the extensive orbital floor defect. The patient underwent orbital floor reconstruction and received intravenous and oral voriconazole. Despite orbital invasion, there were no ophthalmic symptoms or sequelae.
INTRODUCTION
Fungal sinusitis is relatively rare, but its incidence and severity have increased in recent years due to the increase in the prevalence of diabetes, the expanded use of antimicrobial and anticancer drugs for the increasing number of patients with malignant tumors, and the growth in long-term treatment with steroids and immunosuppressants after organ transplantation [1]. When fungal sinusitis invades the orbit, it causes proptosis, chemosis, ophthalmoplegia, retroorbital pain, and vision impairment or blindness depending on optic nerve involvement, as it can result in extensive bony destruction that interrupts the blood supply to the sensory nerve [2]. Herein we present a case of an extensive orbital floor defect due to invasive fungal sinusitis. Despite orbital invasion, there were no ophthalmic symptoms, and the patient’s initial symptoms were limited to right cheek swelling and pain. The patient underwent orbital floor reconstruction with a Medpor Titan surgical implant (Stryker) and was prescribed voriconazole.
CASE REPORT
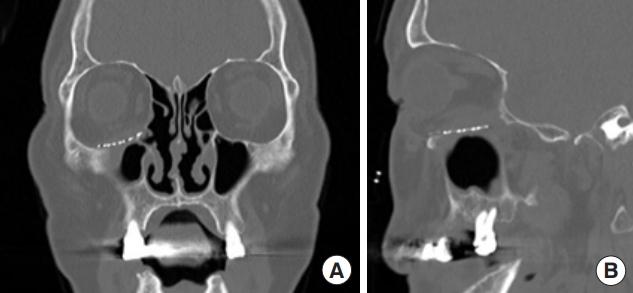
A 62-year-old man visited our clinic due to right cheek pain and swelling that had lasted for 1 month. He had a history of hypertension and recurrent lung adenocarcinoma. He underwent right lower lobectomy 30 months previously and refused adjuvant chemotherapy. After 12 months, mediastinal lymph node enlargement was found, and he received paclitaxel and cisplatin chemotherapy for 5 months. Nine months later, paratracheal metastatic adenocarcinoma was found. He received combined dabrafenib-trametinib chemotherapy, which has been approved for cancers with BRAF mutation, for 4 months, and the facial symptoms appeared. He had hemi-facial swelling and pain, but no ophthalmic symptoms. The patient had never been diagnosed with diabetes, but upon admission, his serum glucose level was 347 mg/dL, a urine glucose test was positive (3+), and his hemoglobin A1c was 11.4%. A computed tomography scan and a Waters’ view of the paranasal sinus showed right maxillary sinusitis with an orbital floor defect (Fig. 1). On hospital day 3, functional endoscopic sinus surgery was performed by the otorhinolaryngology team. Pus-like discharge and fungal impaction were noted (Fig. 2). On a pathologic examination, aspergilloma was noted in necrotic inflammatory exudate that was obtained during exploration. Aspergillus hyphae showing septae with uniform width and dichotomous branching at 45° were observed (Fig. 3).
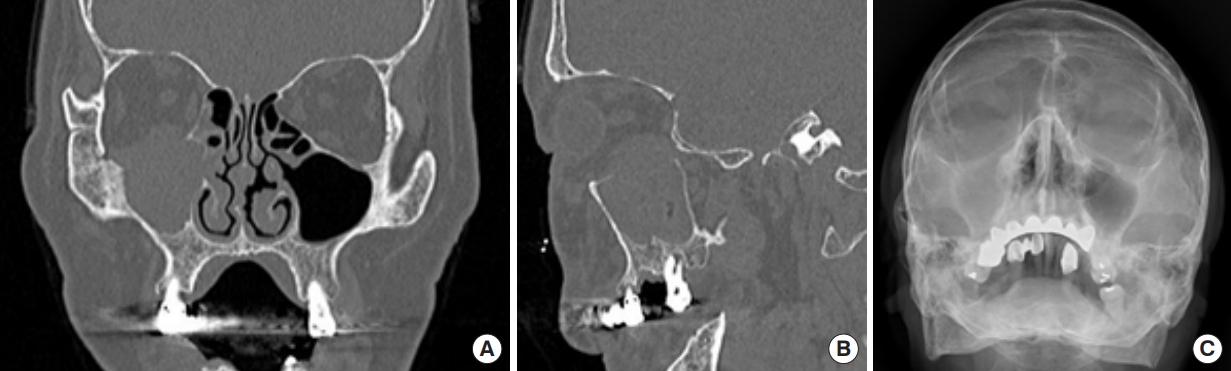
A 62-year-old man with right maxillary sinusitis and orbital floor defect. (A) A computed tomography scan (coronal view). (B) A computed tomography scan (sagittal view). (C) A Waters’ view X-ray.
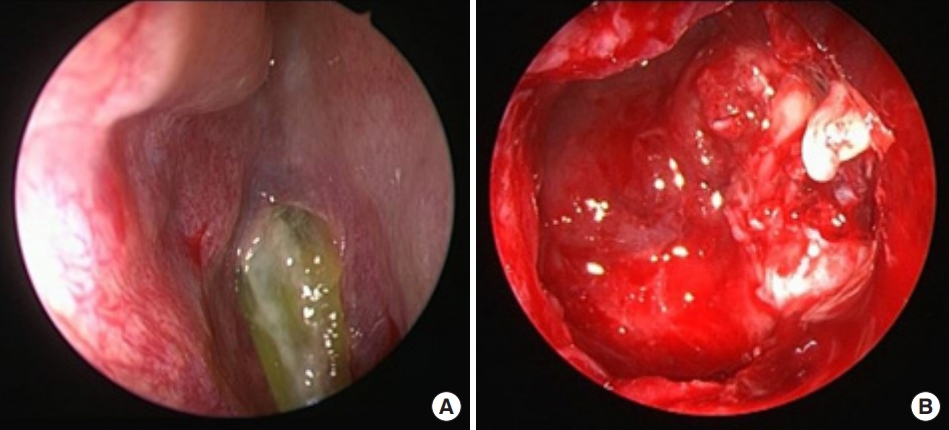
Functional endoscopic sinus surgery was performed by the otorhinolaryngology team. (A) Pus-like discharge. (B) Fungal impaction.

Histopathology of the specimen. Aspergillus hyphae showing septae with a uniform width and dichotomous branching at a 45° angle (hematoxylin and eosin stain, ×400).
On hospital day 7, orbital floor reconstruction with a Medpor Titan surgical implant was done (Fig. 4). Through a subciliary incision. A 2× 2 cm extensive orbital floor defect was noted, and the Medpor Titan surgical implant was tailored to the size of the defect. After fixation with the Medpor Titan surgical implant, successful insertion of the Medpor Titan surgical implant was confirmed via endoscopy. Empirical intravenous ceftriaxone and clindamycin were changed to intravenous voriconazole on postoperative day 8, when the pathology report confirmed aspergilloma. The patient was discharged on postoperative day 18, and there were no ophthalmic symptoms or sequelae.
LITERATURE REVIEW
Invasive fungal sinusitis is a complex disorder that typically manifests as unilateral facial pain and can cause facial bone erosion. Invasive fungal sinusitis should be suspected in immunocompromised patients with acute sinusitis, inflammation of the nasal septal mucosa, unexplained fever or cough, or orbital apex syndrome [3].
Aspergillus is the most common cause of fungal sinusitis, and aspergillosis is classified into invasive and noninvasive infections. Noninvasive infections are either allergic sinusitis or a sinonasal fungal ball, wherein destruction of the sinus mucosa and bony expansion may occur, but without invasion of the tissue or bone. Invasive infections are either localized or fulminant. Localized disease often starts in the sinuses and spreads to adjacent structures through focal bony erosion or even through vessel walls, potentially causing stroke and death. The fulminant form is characterized by multiple organ involvement [4]. Invasive aspergillosis is well documented in immunocompromised patients, with the primary risk factors being neutrophil defects and corticosteroid use. Other predisposing factors include human immunodeficiency virus infection, diabetes mellitus, the use of prosthetic devices or trauma, excessive environmental exposure, and possibly advanced age [4]. Fungi like aspergillus can normally colonize the paranasal sinuses and lungs. Numerous spores are also present in inhaled air. Although an active man can inhale as many as 5.7× 107 aspergillus spores in a day, the incidence of disease is low [4]. Under appropriate conditions, the spores can become saprophytic within a host and multiply, and it is possible for locally aggressive, invasive fungal masses to develop, particularly if the host immunity is severely compromised [5].
Invasive aspergillosis originates from the paranasal sinuses and causes bone destruction, which allows the infection to extend into the apex of the orbit, leading to orbital apex syndrome, and into the cranium, resulting in pachymeningitis or cerebral abscess. It can be fatal and generally has a poor prognosis [3,4,6].
Kawakami et al. [7] reported seven cases of localized invasive sino-orbital aspergillosis. The initial symptoms were reduced blurred vision (57%), unilateral headaches (43%), unilateral abnormal sensations or numbness of the periorbital area (43%), and external ophthalmoplegia (43%). The final visual outcome was no light perception in 86% of the patients, and death related to invasive sino-orbital aspergillosis occurred in 43%.
Contrary to previous studies, in this case, the orbit was invaded and there was an extensive orbital floor defect. However, there were no ophthalmic symptoms or sequelae; the patient’s only symptoms were right cheek swelling and pain. In principle, management of fungal infections often begins with surgical debridement and local irrigation with an antifungal agent. Exceptionally, in this case, to prevent enophthalmos, the patient was treated with debridement and immediate orbital floor reconstruction using a Medpor Titan surgical implant, after which he was prescribed voriconazole. The goal of orbital floor reconstruction is to restore ocular motility and prevent enophthalmos by restoring the native orbital anatomy and volume [8].
For a definitive diagnosis, a histopathologic examination of biopsy specimens with support from the clinical findings and computed tomography appears to be the best modality for the initial examination of patients suspected to have an inflammatory disease or fungal infection [7,9].
DISCUSSION
There is no uniformly accepted, completely effective treatment for invasive sino-orbital aspergillosis. In principle, management of this condition often begins with surgical debridement and local irrigation with an antifungal agent, followed by a systemic antifungal drug [4]. Exceptionally, in this case, debridement and immediate orbital floor reconstruction were performed to prevent enophthalmos caused by the extensive orbital floor defect. The infection was controlled with debridement and an antifungal agent.
In patients with invasive aspergillosis, initial therapy with voriconazole led to better responses and improved survival and resulted in fewer severe side effects than the standard approach of initial therapy with amphotericin B [10]. Herbrecht et al. [11] recommended intravenous voriconazole at a dose of 6 mg/kg body weight twice on day 1, followed by 4 mg/kg for 1 week, and then switching to oral voriconazole 200 mg twice daily for 12 weeks.
Aggarwal et al. [12] reported that no definite treatment protocols existed for orbital aspergillosis, but complete surgical debridement was recommended as the primary treatment in patients with orbital aspergillosis.
In this case, there were no ophthalmic symptoms or sequelae despite orbital invasion. The orbital floor defect was complicated by an erosive, ulcerative lesion and necrotic exudate. Exceptionally, to prevent enophthalmos, this patient was treated with debridement and immediate orbital floor reconstruction with a Medpor Titan surgical implant. Postoperative intravenous voriconazole (400 mg daily for 1 week) and oral voriconazole (200 mg twice daily for 6 months) were effective for infection control and enhanced wound healing.
Notes
Conflict of interest
No potential conflict of interest relevant to this article was reported.
Funding
None.
Ethical approval
The report was approved by the Institutional Review Board of Wonju Severance Christian Hospital (CR323345).
Patient consent
The patient provided written informed consent for the publication and use of his images.
Author contributions
Conceptualization: Jiye Kim. Writing - original draft: Sang Woo Han. Writing - review & editing: Eun Jung Lee, Sug Won Kim, Jiye Kim. Investigation: Sang Woo Han, Min Woo Park, Dong Huan Kwon, Eun Jung Lee. Resources: Minseob Eom, Eun Jung Lee. Supervision: Sug Won Kim, Minseob Eom, Jiye Kim.