 |
 |
- Search
| Arch Craniofac Surg > Volume 24(6); 2023 > Article |
|
Abstract
Background
The traditional nasolabial V-Y advancement flap is widely used for midface reconstruction, particularly for the lower third of the nose and upper lip, as its color and texture are similar to these areas. However, it provides insufficient tissue to cover large defects and cannot restore the nasal convexity, nasal ala, and adjacent tissues. The purpose of this study is to investigate the modified nasolabial V-Y advancement flap with extension limbs the along alar crease for the reconstruction of complex midface defects.
Methods
A retrospective analysis of 18 patients, who underwent reconstruction with the modified nasolabial V-Y advancement flap, was performed between September 2014 and December 2022. An extension limb was added along the alar crease, adjacent to the defect area, and was hinged down as a transposition flap at the end of the advancement flap.
Defects of the lower third of the nose and upper lip are particularly challenging for the reconstructive surgeon. Interwoven concavities, convexities, and skin thickness variation in the lower third of the nose make its reconstruction difficult [1]. The appropriate reconstruction option for midface defects is based on several variables, including defect location, size, and extent, and involvement of adjacent subunits [2].
Nasolabial flaps are ideal for reconstructing midface defects, including those of the lower third of the nose and upper lip. Optimal outcomes may be achieved using superiorly based nasolabial flaps. It is important to place the scar within the nasolabial fold by designing the lower border of the flap to correspond with the deepest point of the nasolabial fold. Accurate flap division and insetting allow excellent alar and tip reconstruction, particularly for full-thickness defects that require cartilage replacement. Traditional nasolabial flaps are usually divided after 3 weeks. The main disadvantages of the superiorly based nasolabial flap are the need for two operations and compromised results in complex defects [3].
Nasolabial V-Y advancement flap has gained popularity for midface reconstruction because it is easy to perform as a single operation, has excellent vascularity, produces an inconspicuous donor scar, does not distort facial features, and offers an excellent color and texture match [4]. However, its pedicle has limited mobility that allows only rotation or advancement and may not provide satisfactory outcomes for complicated and multiple subunit defects [5-7]. Limited mobility of the nasolabial V-Y advancement flap results in tension and distortion of the facial structures when such a flap is used [8]. In particular, these flaps cause severe distortion when used for ala area coverage [4].
According to previous papers, the extension limb modification of the traditional nasolabial V-Y advancement flap allowed successful reconstruction of complex defects of the lower third of the nose and the upper lip [6-8]. The modification of the traditional nasolabial flap provided sufficient tissue to cover large defects without severe distortion. However, the disadvantage of the extension limb is that the scar can be longer than the traditional nasolabial flap. In order to overcome this, we devised that the extension limb was placed along the alar crease to increase the tissue quantity and to hide the scar. The present study assessed the alar crease as a donor site of the extension limb in nasolabial V-Y advancement flaps.
The study protocol conformed to the Declaration of Helsinki and was approved by the Institutional Review Board of Chungnam National University Hospital (IRB No. 2022-05-089). Written informed consent was obtained from all patients. We performed a retrospective chart review of 18 patients, including 11 women and seven men, who underwent Mohs micrographic surgery for skin cancer (17 basal cell carcinoma and 1 squamous cell carcinoma), followed by midface defect repair using the modified nasolabial V-Y advancement flap, between September 2014 and December 2022. The mean age was 71.1 years (range, 51â91 years).
A V-Y advancement flap, centered on the nasolabial crease, was designed. The base of the triangular skin flap abutted the lower border of the defect and the alar crease, whereas the apex reached up to the oral commissure within the nasolabial crease. The flap vector was parallel to the nasolabial crease with an extension limb along the alar crease. The extension limb was hinged down as a transposition flap. The location, size, and number of extension limbs were adjusted according to the defect. For upper lip defects, the extension limb was added on the lateral side of the flap, along the lateral part of the alar crease (Figs. 1A, 2). For alar or medial cheek defects, the extension limb was placed on the medial side of the flap, along the lower part of the alar crease adjacent to the upper lip (Figs. 1B, 3). In cases with large or complex defects including the alar rim, bilateral extension limbs were used (Figs. 1C, 4).
A skin incision was made and the planned V-Y advancement flap was elevated. The flap was released on all sides, leaving it attached to the muscle only at its center. The distal part of the flap and the extension limb were elevated in the subdermal plane. The extension limb was thinned from the alar crease. In the proximal two-thirds of the flap, the orbicularis oris muscle was kept above the plane of dissection and the branches of facial, superior labial, and angular arteries were carefully preserved to maintain the blood supply to the flap. The flap was advanced into the defect and the extension limb along alar crease was hinged at its base for transposition. Care was taken to avoid excessive tension during flap insetting.
Defect sizes ranged from 1.5Ă 1.5 cm to 4.0Ă 3.0 cm (Table 1). Lateral extension limb was used in 11 cases with upper lip defects, while a medial extension limb was used in four cases with alar or medial cheek defects. Bilateral extension limbs were used for large (patient 3) and complicated defects involving the alar rim (patient 12). The average follow-up after surgery was 11.6 months (Table 1) [6].
The complication rate was 33.3% (6/18), including two cases of temporary paresthesia and one case each of temporary flap congestion and temporary nostril deformity. One patient developed permanent nostril asymmetry, but opted not to have it corrected, while another developed partial flap necrosis that resolved with conservative treatment. Flap texture, color, and thickness were similar to those of the surrounding tissues and satisfactory aesthetic outcomes were achieved in all 18 patients (Table 1).
The excellent subcutaneous blood supply of V-Y advancement flaps makes them ideal for facial reconstruction. They do not leave dog ears, have excellent cosmesis, and avoid tension, which makes them superior to rotation flaps, skin grafts, and primary closure. This is particularly true for midface defects because V-Y nasolabial flaps provide ample tissue with excellent vascularity and mobility. Moreover, they can be designed without concern for the pedicle width. They also allow primary closure of the donor site and produce inconspicuous scars [4].
However, reconstruction of large and complicated defects using nasolabial V-Y advancement flaps presents a reconstructive challenge. Various modifications have been suggested to allow closure of larger defects and obtain greater advancement. Chan [9] suggested direct undermining of the flap to achieve greater advancement. Pribaz et al. [8] added an extension limb to the advancing edge of the flap, allowing effective reconstruction of defects that could not be reconstructed using the traditional nasolabial flap. In the present study, we reconstructed large and complicated midface defects using nasolabial V-Y advancement flaps by including an extension limb along alar crease.
The nasolabial flap is appropriate for the reconstruction of most upper lip defects. Nasolabial flap options for large defects include transposition, cheek advancement, tunneled subcutaneous pedicle transposition, and island pedicle flaps [10,11]. The disadvantages of the first three of these include nasolabial fold distortion or ablation and lack of moustache hair in men. The subcutaneous island pedicle flap can be used to close large upper lip defects and can provide facial hair [12]. In the present study, an extension limb lateral to the ala was used for the reconstruction of upper lip, alar base, and nostril floor. The donor scar from the extension limb was concealed in the alar crease. The portion of the extension limb under the alar base was deepithelialized to form a platform at the alar base. The nostril floor and upper lip were reconstructed using non-hair-bearing tissue adjacent to the ala (Fig. 2).
Repair of alar and nasolabial fold defects is also challenging [13], but the nasolabial V-Y advancement flap is a good option in these cases. In the present study, a medial extension limb along the lower alar crease was used to repair large defects without excessive mobility (Fig. 3).
For larger defects of the ala and nasolabial fold (Fig. 4), bilateral extension limbs were used. Medial and lateral extension limbs were positioned along the lower alar crease and lateral to the defect, respectively. A nasal conformer was used for 2 months postoperatively to correct nostril asymmetry. Longterm postoperative follow-up showed satisfactory aesthetic results, with the exception of nostril asymmetry.
For complicated defects involving the alar rim (patient 9) [6], the extension limbs were placed at the lateral aspect of the alar crease and upper lip, which covered the alar rim, alar base, and nostril floor. The donor scar from the extension limb was concealed in the alar crease. A full-thickness alar rim defect was reconstructed by turning the extension limb away along the alar crease. The base of the flap was advanced to cover the alar base. The nostril floor was reconstructed using non-hair-bearing tissue from the upper lip extension limb.
This study has a few limitations. The number of patients in the study is relatively small, making it challenging to generalize the results of our procedures. Consequently, we did not quantify the complexity and size of a defect that can be reconstructed with extension limbs. Further analysis is necessary to determine how complex and large defects can be reconstructed without causing structural distortion to adjacent tissues by increasing the number of patients.
In conclusion, the nasolabial V-Y advancement flap with an extension limb along alar crease may be used to reconstruct large and complicated midface defects. This modified method provides sufficient tissue to cover large defects and restore the nasal convexity, nasal ala, and adjacent tissues to prevent structural distortion of the nose and upper lip. Also, the donor scar from the extension limb can be easily concealed in the alar crease. The alar crease was found to be an acceptable donor site for the reconstruction of large and complex nasal and upper lip defects.
Notes
Funding
This work was supported by the Research fund of Chungnam National University and the Korea Health Technology R&D Project through the Korea Health Industry Development Institute, funded by the Ministry of Health & Welfare, Republic of Korea (grant no.: HI20C2088).
Ethical approval
The study was approved by the Institutional Review Board of Chungnam National University Hospital (IRB No. 2022-05-089) and performed in accordance with the principles of the Declaration of Helsinki. The informed consent was waived because this study design is a retrospective chart review.
Fig. 1.
Illustration of the modified nasolabial V-Y advancement flap. (A) Lateral extension limb used nasolabial V-Y advancement flap. A, a portion of the V-Y advancement flap; L, a portion of the lateral extension limb from the lateral part alar crease for covering the nostril floor and upper lip defect. (B) Medial extension limb used nasolabial V-Y advancement flap. A, a portion of the V-Y advancement flap; M, a portion of the medial extension limb from the along lower part of alar crease for covering the medial cheek defect. (C) Bilateral extension limb used nasolabial V-Y advancement flap. A, a portion of the V-Y advancement flap; L, a portion of the lateral extension limb from the along upper part of alar crease and M, a portion of the medial extension limb from the along lower part of alar crease for covering the larger defects of the ala and nasolabial fold.
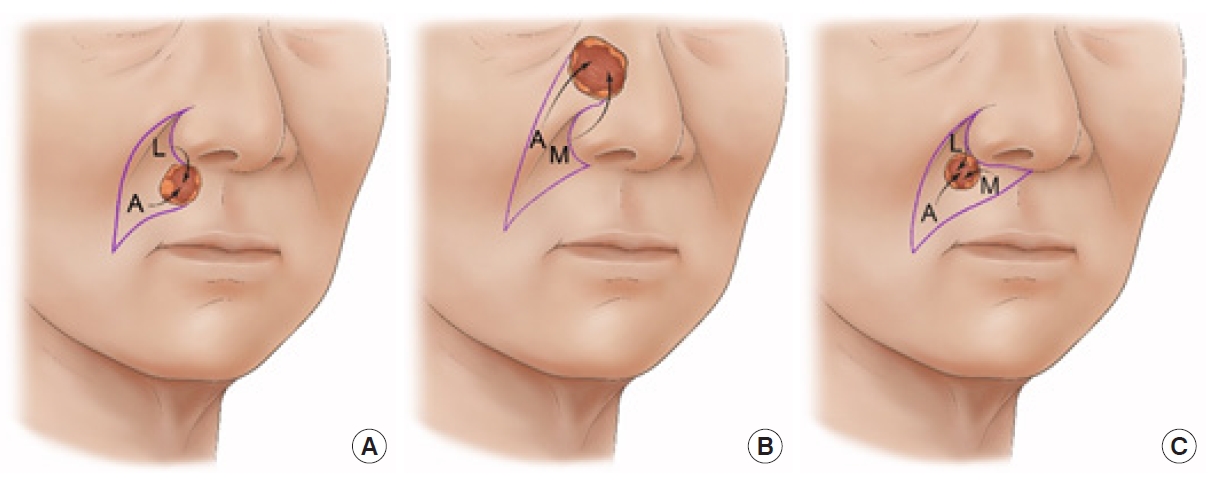
Fig. 2.
A 65-year-old man (patient 9) with a 2.2Ă2.2 cm defect of the right upper lip and alar base following Mohs micrographic surgery. (A) Preoperative photograph. (B) Modified nasolabial V-Y advancement flap design including a lateral extension limb along the lateral alar crease (red arrow). (C) Immediate postoperative view. (D) A 5-month postoperative view. Compared to preoperative, there is little distortion of the nasal ala and upper lip. The donor scar arising from the lateral extension limb from the lateral part alar crease was concealed by alar crease (red arrow).

Fig. 3.
A 68-year-old woman (patient 18) with a 2.5Ă3.5 cm defect of the right medial cheek and nasal base following Mohs micrographic surgery. (A) Preoperative photograph. (B) Modified nasolabial V-Y advancement flap design including a medial extension limb along the lateral to lower alar crease (red arrow). (C) Immediate postoperative view. (D) A 2-month postoperative view. Compared to preoperative, there is little distortion of the medial cheek and nasal ala. The donor scar arising from medial extension limb from the along lower part of alar crease was concealed by alar crease (red arrow).

Fig. 4.
A 91-year-old woman (patient 3) with a 4.0Ă3.0 cm defect of the left ala and nasolabial fold following Mohs micrographic surgery. (A) Preoperative photograph. (B) Modified nasolabial V-Y advancement flap design including extension limbs along the lower alar crease (Medial extension limb, red arrow) and lateral to the defect (Lateral extension limb). (C) A conformer was applied for 2 months to correct nostril asymmetry. (D) A 2-month postoperative view. Compared to preoperative, there is little distortion of the nasal ala. The donor scar arising from the medial extension limb from the along lower part of alar crease was concealed by alar crease (red arrow).
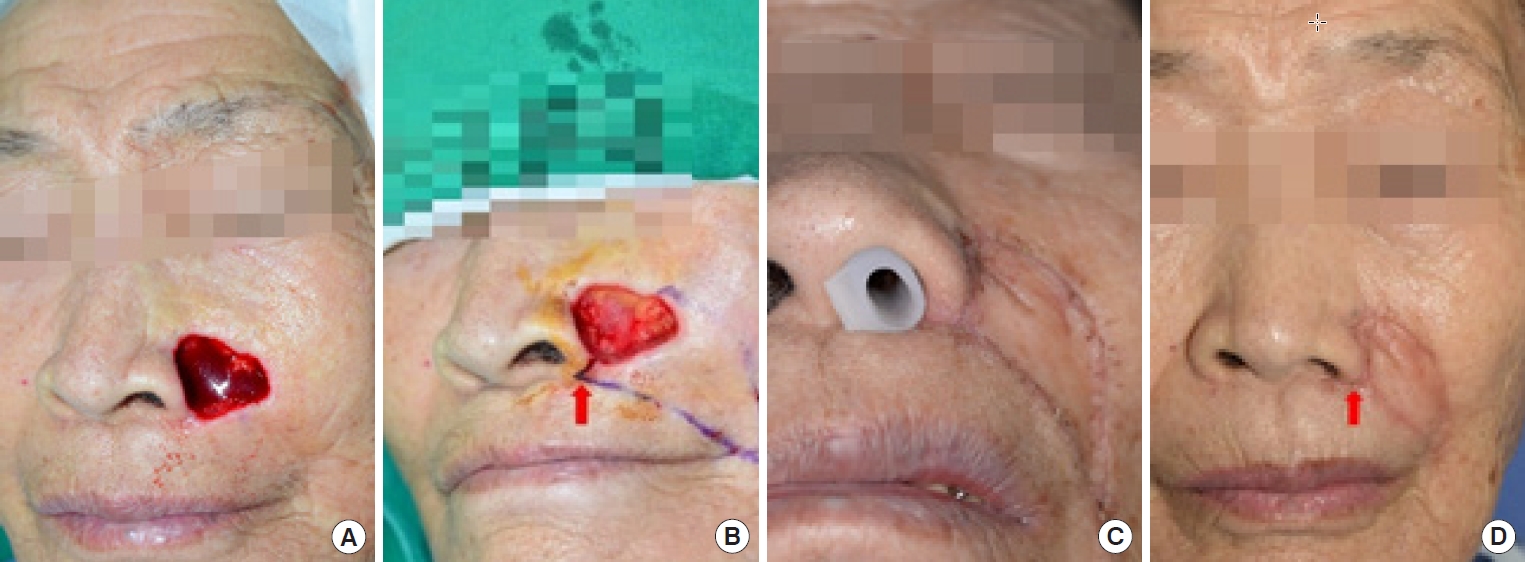
Table 1.
Clinical characteristics
REFERENCES
1. Kim MJ, Lim H, Park DH. Current strategies for aesthetic soft tissue refinement in nasal reconstruction. Arch Craniofac Surg 2022;23:95-102.




3. Lee DW, Ryu HR, Choi HJ, Kim JH. One-stage reconstruction of full-thickness alar defects with a folded nasolabial island flap. Arch Craniofac Surg 2021;22:296-302.




4. Yildirim S, Akoz T, Akan Md, Avci G. Nasolabial V-Y advancement for closure of the midface defects. Dermatol Surg 2001;27:656-8.


5. Li JH, Xing X, Liu HY, Li P, Xu J. Subcutaneous island pedicle flap: variations and versatility for facial reconstruction. Ann Plast Surg 2006;57:255-9.

6. Oh SK, Song B, Lee WS, Oh SH. Repair of a nasal ala defect involving the alar rim and nostril floor. Dermatol Surg 2023;49:411-3.


7. Chun K, Lee CL, Yang HJ, Oh SH. Repair of a large upper lip defect involving the alar base and nostril floor. Dermatol Surg 2021;47:1634-5.


9. Chan ST. A technique of undermining a V-Y subcutaneous island flap to maximise advancement. Br J Plast Surg 1988;41:62-7.


10. Zitelli JA, Brodland DG. A regional approach to reconstruction of the upper lip. J Dermatol Surg Oncol 1991;17:143-8.


11. Skouge JW. Upper lip repair: the subcutaneous island pedicle flap. J Dermatol Surg Oncol 1990;16:63-8.









