|
 |
- Search
| Arch Craniofac Surg > Volume 25(1); 2024 > Article |
|
Abstract
Background
This study analyzed the demographic characteristics of patients with facial palsy who were treated using either dynamic or static procedures. This study aimed to compare the frequency of procedure implementation and age distribution between the two groups.
Methods
This study retrospectively analyzed the medical records of patients treated for facial palsy at a single institution from 2014 to 2022. Among cases included in our study, dynamic procedures involved cross-facial nerve graft and latissimus dorsi or gracilis muscle flap transfer. Static procedures included gold weight insertion, canthopexy, browlift, and thread lift/static slings.
Results
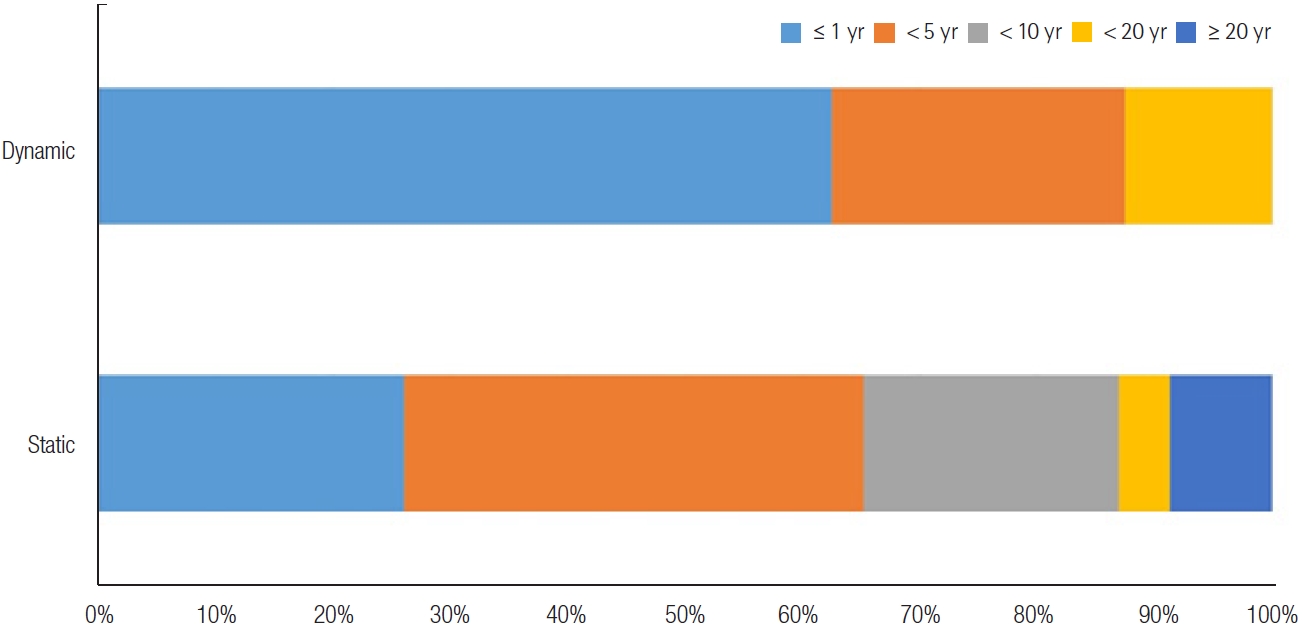
Among the 31 patients included in our study, eight (25.8%) incorporated dynamic techniques, and the average age of patients was 44.75 years (range, 24ŌĆō68 years) with a male to female ratio of 1:4. The remaining 23 patients (74.2%) underwent a static procedure, of which the average age was 59.17 years (range, 23ŌĆō81 years) which was statistically significantly higher than the average age of 44.75 of dynamic patients (p= 0.013). Regarding the timing of treatment after diagnosis, no patient underwent dynamic procedures more than 20 years after initial diagnosis. A greater diversity in the timing of treatment was observed in the static group. All patients who underwent dynamic procedures were treated using static procedures during the study period.
Conclusion
Because aesthetics-based static techniques are typically quick outpatient procedures that can be performed under local anesthesia, our study shows that these are often preferred treatments for all age groups, especially for debilitated or older patients. Further research is required to investigate the long-term functional outcomes of these surgical techniques in a wider population of patients.
Facial palsy can have over 50 etiologies, including infectious, traumatic, neoplastic, neurological, congenital, and systemic causes [1]. The variety of etiologies can make the management of facial palsy challenging. Although facial paralysis is not a life-threatening disease, it is a debilitating condition with functional, aesthetic, and psychological consequences. Symptoms related to facial expression include ectropion of the eyelids or lagophthalmos, which leads to corneal exposure, tearing, and potential vision loss [2]. Paralysis of the orbicularis oris muscle paralysis results in oral incompetence.
A wide variety of techniques have been developed for facial reanimation and improvement of functional problems [3]. Multiple surgical interventions combining both dynamic and static approaches are usually required to achieve optimal results [4]. Though dynamic procedures are generally known to have better, longer-lasting results, the static approach is usually preferred for elderly patients and those who desire minor revision.
Treatment of facial palsy remains complex, with no generally established algorithm for surgical intervention in the literature. We aimed to analyze the demographics of patients with facial palsy treated with different techniques.
This retrospective study analyzed the medical records of patients treated for facial palsy at a single institution between January 2014 and December 2022. This study was approved by the Institutional Review Board of Yonsei University Gangnam Severance Hospital (IRB No. 2023-1012-001). The requirement for informed consent from the patient was waived. The patient demographics included age, sex, etiology of facial palsy, and treatment initiation. Treatment initiation refers to the period from the time when facial paralysis is diagnosed to the time when surgical procedures are performed.
The surgical procedures were divided into two categories: dynamic and static. The dynamic procedure involved a cross-facial nerve graft and latissimus dorsi or gracilis muscle flap transfer. Static measurements included gold weight insertion, canthopexy, browlift, and thread lift/static slings (Table 1).
The two groups were identified and compared based on the type of procedure. As this was a retrospective study conducted over many years, the techniques chosen varied, and no standard algorithm has been applied to determine the optimal treatments for patients. All procedures in the two groups were performed by a senior author.
All statistical analyses were performed using SPSS version 29 (IBM Corp.). The demographic information of the two subgroups (dynamic procedure group versus static procedure group) was compared using the Fisher exact test for categorical variables and the Mann-Whitney U test or independent t-test for continuous variables. For each scale, we report the mean and standard deviation of the scores. Statistical significance was considered at p < 0.05.
The etiologies include idiopathic, infectious, and iatrogenic causes. Iatrogenic causes accounted for the highest number of cases (n = 23, 74.2%). Resection of acoustic neuromas and schwannomas was the most common iatrogenic etiology. Idiopathic BellŌĆÖs palsy was the second most common cause of facial palsy (n = 7, 22.6%). One patient had a herpes zoster infection (Table 1).
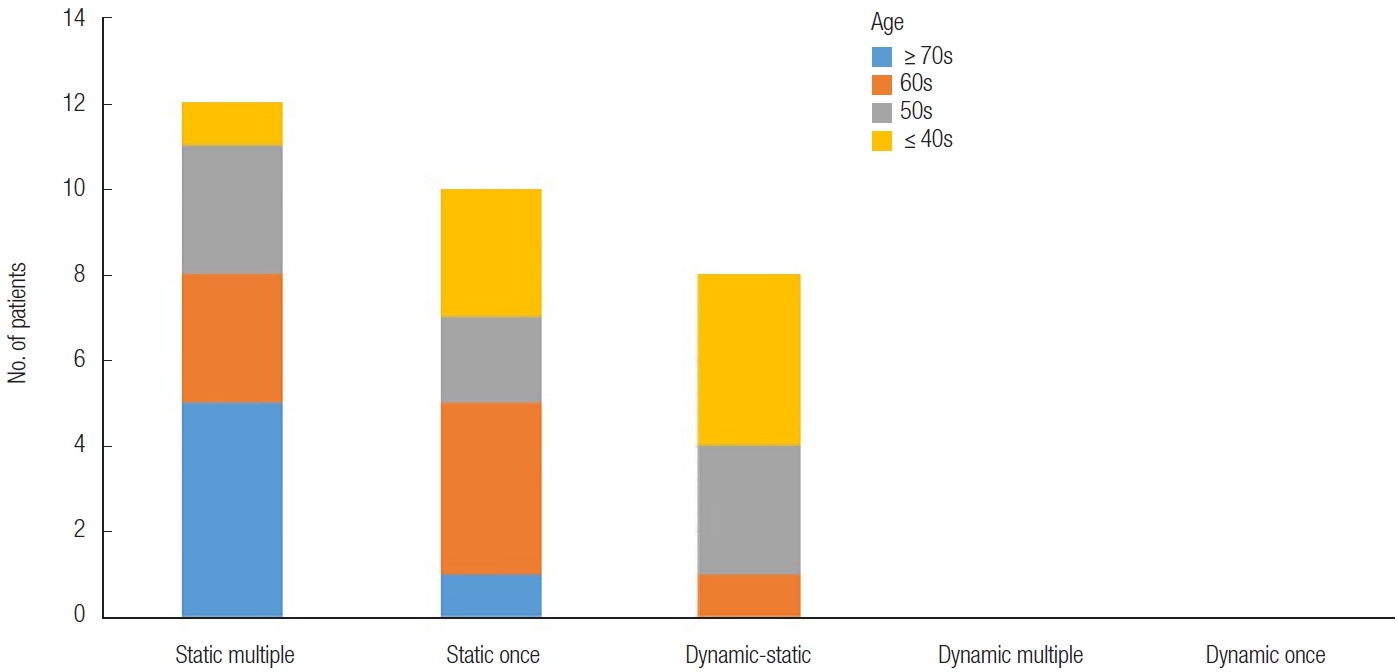
A total of 31 patients were included in this retrospective review, comprising 22 females and nine males, from 23 to 81 years of age at the time of the procedure (mean, 55.37 years). The patients were divided into two groups according to the type of procedure. Eight patients (25.8%) underwent dynamic techniques, and the remaining 23 (74.2%) underwent static procedures only. There was no significant difference in sex between the two groups (p = 0.771). The mean age of the dynamic procedure group was 44.75 years (range, 24ŌĆō68 years) and was lower than the 59.17 of the static cohort (range, 23ŌĆō81 years; p = 0.013) (Table 2). The age distributions of the two groups are shown in Fig. 1. No patients aged more than 70 years were included in the dynamic group and diverse age distributions were identified in the static group.
Among the eight (25.8%) patients who underwent dynamic techniques, two patients underwent multiple dynamic procedures and subsequent or simultaneous static techniques. A 28-year-old woman underwent simultaneous neurovascular free gracilis muscle transfer, cross-facial nerve grafting, and lateral canthopexy. The other was a 41-year woman who underwent a cross-facial nerve graft and gold plate insertion simultaneously, was treated with a neurovascular latissimus dorsi muscle free flap transfer 2 years later. She also underwent lateral canthopexy 3 years after the initial treatment for lagophthalmos.
The frequency of implementation in the two groups is detailed in Fig. 2. None of the patients underwent dynamic procedures alone. In other words, all eight patients who underwent dynamic procedures were treated with static procedures within the study period. Twelve patients (38.7%) underwent multiple static techniques, and 10 patients (32.3%) underwent static techniques once.
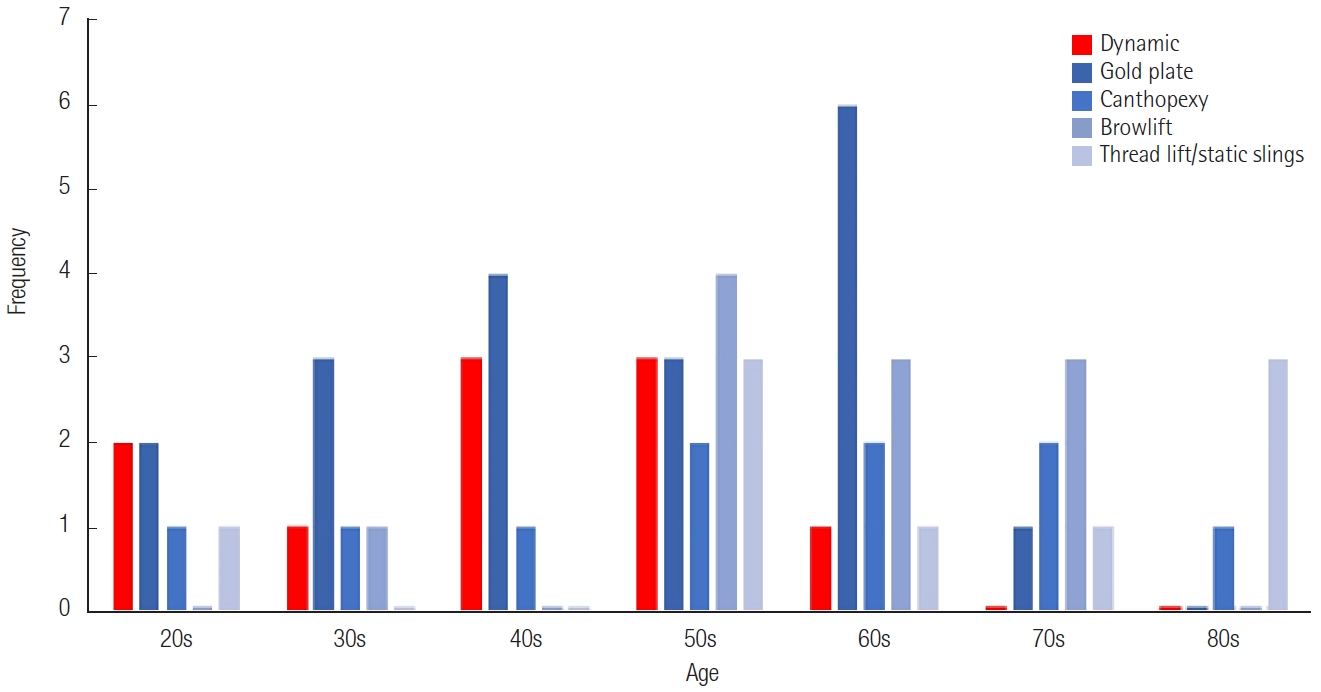
A total of 59 procedures were performed for facial palsy patients with facial palsy. Among the 10 dynamic procedures, the cross-facial nerve graft was the most implemented procedure (n = 6, 60%). Static procedures were performed 49 times for patients with facial palsy: 19 cases of gold weight insertion, 10 cases of canthopexy, 11 cases of browlift, and nine cases of thread lift/static slings (Table 3).
For the timing of treatment initiation after diagnosis in the dynamic group, 62.5% of patients underwent procedures within a year and 25.0% underwent procedures within 5 years. None of the patients underwent dynamic procedures more than 20 years after developing facial palsy. In the static group, 26.1% of the patients underwent procedures within a year, 39.1% within 5 years, 21.7% within 10 years, and 8.7% at over 20 years. Fig. 3 indicates a greater diversity in the timing of treatment initiation in the static group.
The treatment of facial paralysis is complex, and any surgical intervention must carefully consider the patientŌĆÖs age, medical history, expectations, and risk tolerance [1]. Surgical facial reanimation is a process rather than a single procedure. Numerous surgical options have been introduced and applied, depending on the duration of the facial palsy. The duration of paralysis is paramount as it is an indicator of the viability of the existing facial mimetic muscles and motor nerve terminal branches, which are necessary for potential reinnervation [5,6]. Acute paralysis within 3 weeks can be managed with facial nerve decompression or repair. Nerve transfer procedures are appropriate for intermediate facial paralysis. For chronic paralysis due to facial muscle atrophy, regional or free muscle transfer can be used. Static techniques for facial reanimation can be used during the acute, intermediate, or chronic phases of facial paralysis [7,8].
The dynamic reanimation procedures in this study included cross-facial nerve graft and free muscle transfer using the latissimus dorsi and gracilis muscles. Among the four patients who received free muscle transfer, three patients (75%) were aged less than 50 years. Many studies advocate the treatment goal of facial palsy be true ŌĆ£reanimationŌĆØ or facial movement, thereby supporting dynamic procedures wherever possible [9,10]. Stephan who compared dynamic and static procedures for treating paralytic eyelids, confirmed that dynamic procedures confer significantly better improvements in eyelid symptoms and blink restoration [11]. Iseli et al. [12] proposed that dynamic reconstruction has more advantages than static reconstruction, even for malignant pathologies or radiotherapy. However, as dynamic approaches are inherently more complex procedures with longer operative times and higher intraoperative complication rates for high-risk and elderly patients, static approaches are favored under certain circumstances.
Static techniques have significant benefits that can provide an alternative to or enhance the results of dynamic procedures. Static procedures offer shorter surgical time and immediate results. In addition, they are useful for treating temporary facial paralysis when nerve recovery is expected [13]. Static procedures are ideal for patients who cannot tolerate dynamic reconstruction because of poor health or age [14]. Gold weight insertion, canthopexy, brow lift, and threaded lift/static slings were included in this study. The mean age of the patients who underwent static procedures was significantly higher than that of the patients who underwent dynamic procedures. In addition, the age distribution of patients involved in static procedures was more diverse, ranging from 23 to 81 years.
Compared to previous studies that have focused on diagnostic methods, existing surgical methods, or introduction of novel techniques, this study focused on the demographic characteristics of patients with facial palsy who were treated with different types of procedures. This study demonstrated that the age distribution of patients who underwent a rather invasive dynamic procedure was lower than that of patients who underwent static procedures. Owing to the quick and immediate nature of static procedures, all patients who underwent dynamic procedures underwent static procedures to achieve better aesthetic outcomes with a lower burden. In conclusion, static procedures are preferable for various age groups, especially debilitated or older patients.
This study had several limitations. The number of patients surveyed was small, the study was conducted at a single institution, and the study design was retrospective. Moreover, postoperative aesthetic results and complications were not included in this study. Future studies with multicenter retrospective designs are needed to compare the surgical outcomes and complications of dynamic and static procedures.
Notes
Ethical approval
The study was approved by the Institutional Review Board of Gangnam Severance Hospital (IRB No. 2023-1012-001) and performed in accordance with the principles of the Declaration of Helsinki. Written informed consent was obtained. The requirement for informed consent from the patient was waived.
Table┬Ā1.
Etiologies of facial paralysis
Table┬Ā2.
Patient demographics
Table┬Ā3.
Listing of dynamic and static techniques for facial paralysis treatment
REFERENCES
1. Melvin TA, Limb CJ. Overview of facial paralysis: current concepts. Facial Plast Surg 2008;24:155-63.


2. Park H, Jeong SS, Oh TS. Masseter nerve-based facial palsy reconstruction. Arch Craniofac Surg 2020;21:337-44.




3. Koo WY, Park SO, Ahn HC, Ryu SR. Facial reanimation using the hypoglossal nerve and ansa cervicalis: a short-term retrospective analysis of surgical outcomes. Arch Craniofac Surg 2021;22:303-9.




4. Nadol JB, McKenna MJ. Surgery of the ear and temporal bone. Lippincott Williams & Wilkins; 2005.
5. Garcia RM, Hadlock TA, Klebuc MJ, Simpson RL, Zenn MR, Marcus JR. Contemporary solutions for the treatment of facial nerve paralysis. Plast Reconstr Surg 2015;135:1025e-1046e.


6. Harris BN, Tollefson TT. Facial reanimation: evolving from static procedures to free tissue transfer in head and neck surgery. Curr Opin Otolaryngol Head Neck Surg 2015;23:399-406.

8. Hohman MH, Hadlock TA. Etiology, diagnosis, and management of facial palsy: 2000 patients at a facial nerve center. Laryngoscope 2014;124:E283-93.


9. Bergeron CM, Moe KS. The evaluation and treatment of upper eyelid paralysis. Facial Plast Surg 2008;24:220-30.


10. Douglas RS, Gausas RE. A systematic comprehensive approach to management of irreversible facial paralysis. Facial Plast Surg 2003;19:107-12.


11. Morley SE. ŌĆśAre dynamic procedures superior to static in treating the paralytic eyelid in facial paralysis?ŌĆÖ. J Plast Reconstr Aesthet Surg 2023;77:8-17.


12. Iseli TA, Harris G, Dean NR, Iseli CE, Rosenthal EL. Outcomes of static and dynamic facial nerve repair in head and neck cancer. Laryngoscope 2010;120:478-83.


- TOOLS
-
METRICS

-
- 0 Crossref
- Scopus
- 972 View
- 36 Download
- Related articles in ACFS
-
Simple Aesthetic Correction for Patients with Acute Auriculocephalic Angle2015 April;16(1)