Surgical management of severe cherubism persisting into early adulthood: a case report and literature review
Article information
Abstract
Cherubism is a rare fibro-osseous condition characterized by bilateral expansion of the mandible and maxilla. Due to its rarity, treatment guidelines for cherubism have not been clearly established. Observation without surgical intervention is typically recommended, as cherubism often regresses spontaneously after puberty. However, a surgical intervention may be necessary if aggressive lesions lead to severe complications. In this report, we present a case involving surgical management of cherubism that did not spontaneously regress until early adulthood. An 18-year-old man was diagnosed with cherubism, presenting characteristic upward-looking eyes and a swollen face. He strongly desired surgical management. Gross contouring of the mandible was performed using an osteotome. Subsequently, delicate contouring was performed by bone burring and curettage. The remaining multiple locular bony defects were filled with demineralized bone matrix. No major complications, including infection and hematoma, occurred during the 8-month follow-up period. The facial contour remained stable without the aggravation of cherubism. The patient was satisfied with the cosmetic results. Considering that cherubism is a rare disease globally, with few reported cases in Korea, and that treatment guidelines are not clearly established, we anticipate that the results of this case will contribute to the development of future protocols for treating cherubism.
INTRODUCTION
Cherubism is a rare autosomal-dominant fibro-osseous condition [1]. This benign disorder leads to symmetrical, progressive swelling of the jaw, primarily affecting the mandible, during childhood [2]. The condition is caused by mutations in the SH3 domain-binding protein 2 (SH3BP2) gene, with approximately 50% of cases resulting from de novo mutations that occur without any family history [3]. Clinically, cherubism is characterized by symmetrical bilateral swelling of the mandible, as opposed to the maxilla [4]. The diagnosis relies on a combination of the characteristic clinical presentation, imaging findings, histological evidence, and the identification of a heterozygous pathogenic variant in SH3BP2 through molecular genetic testing. Imaging typically reveals an expanded bone structure with multilocular radiolucency, a coarse trabecular pattern, and cortical bone thinning [5,6].
Conservative treatment is typically recommended for cherubism, as the condition usually manifests between the ages of 2 and 7 and often regresses spontaneously after puberty [4]. However, surgical intervention may be considered if the deformity is associated with significant enlargement of the jaw that necessitates cosmetic correction, impairs breathing and swallowing, or interferes with tongue movement [4]. Some studies indicate that early surgical intervention during the disease course can prevent long-term sequelae, potentially obviating the subsequent need for more complex reconstructive surgery [2]. Cherubism is a rare condition, and the guidelines for its surgical management remain a subject of debate.
We report a rare case of cherubism that did not regress spontaneously in early adulthood. The patient was treated with bilateral shaving of the mandibular body, angle, and ramus, which resulted in satisfactory cosmetic improvement.
CASE REPORT
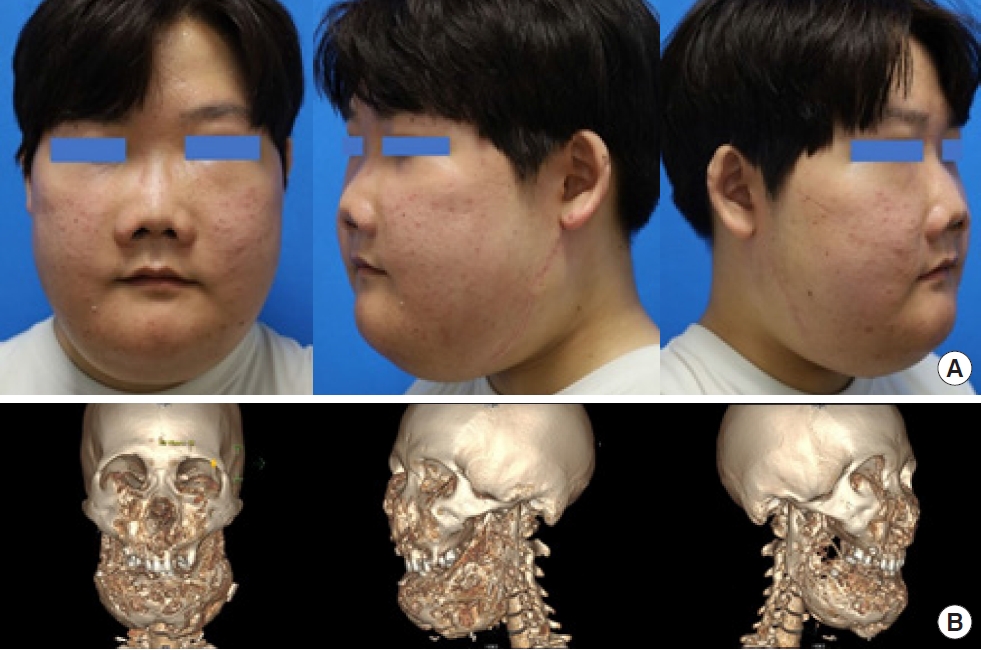
An 18-year-old man presented to the department of plastic and reconstructive surgery on March 8, 2023, seeking cosmetic improvement (Fig. 1). His parents first observed that his cheeks were bulging when he was around 6 or 7 years old. The patient has experienced symptoms of nasal obstruction since the age of 8. He consulted an otolaryngologist for the removal of fibrous tissue associated with nasal cavity cherubism and subsequently underwent endoscopic sinus surgery.

An 18-year-old man was diagnosed with cherubism, presenting characteristic upward-looking eyes and a swollen face.
Despite the expectation that the cosmetic issues caused by the enlarged jaw would improve after puberty, the cherubism of the mandible did not spontaneously regress in early adulthood. Therefore, the patient was referred to the department of plastic and reconstructive surgery for surgical treatment.
Due to early exfoliation of the deciduous teeth, the patient retained only nine upper and four lower teeth, including a mobile left lower lateral incisor, and exhibited severe malocclusion (Fig. 1). He presented with orbital globe elevation and narrowing of the orbit, characteristic of cherubism, as well as generalized facial swelling extending from both cheeks to the chin. Preoperative computed tomography revealed bilateral “soap bubble” appearance lesions with bulging contours and cortical thinning in both the mandible and maxilla, as well as an expansile mass effect on both orbits (Fig. 2). A multilocular, radiolucent, coarse trabecular pattern of expansile remodeling was observed in the bilateral body, angle, ramus, and coronoid process of the mandible, resulting in cortical thinning.
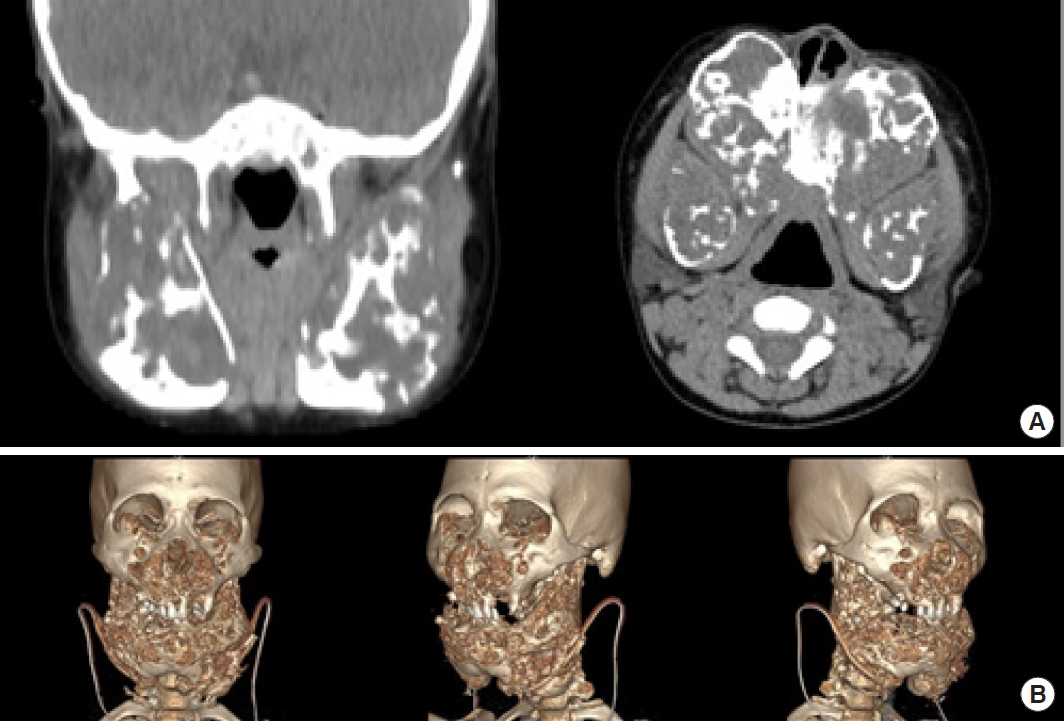
Preoperative computed tomography revealed bilateral “soap bubble” appearance lesions with bulging contours and cortical thinning in both the mandible and maxilla, as well as an expansile mass effect on both orbits. (A) Photograph at age 8. (B) Photograph at age 20.
Considering the patient’s strong desire for surgery and the progressive nature of the condition, which had not improved by early adulthood, the decision was made to perform surgery to contour the mandible. While there are studies suggesting that medications like calcitonin can prevent the inhibition of bone resorption, the lesion has already advanced to a stage where the patient prefers a surgical alteration to their facial appearance.
Under general anesthesia, a tracheostomy was performed to secure the operative field. An incision was made from the menton to the bilateral gonion, with flap elevation both inferiorly and superiorly to the suprafascial layer. A horizontal incision was then created in the belly of the platysma muscles on both sides, and dissection was carried out using a periosteal elevator to expose the bilateral rami of the mandible (Fig. 3). Gross contouring of the bilateral body, angle, and ramus of the mandible was achieved using an osteotome, while delicate contouring was accomplished with a bone burr and curettage (Fig. 3). Due to the weakened state of the condylar neck and bones, extensive use of the osteotome was avoided to reduce the risk of breakage; instead, the shaving method was primarily utilized. Demineralized bone matrix was used to fill multiple locular bone defects that remained after contouring through osteotomy and bone burring (Fig. 3). A compressive dressing was applied using a Barton bandage.
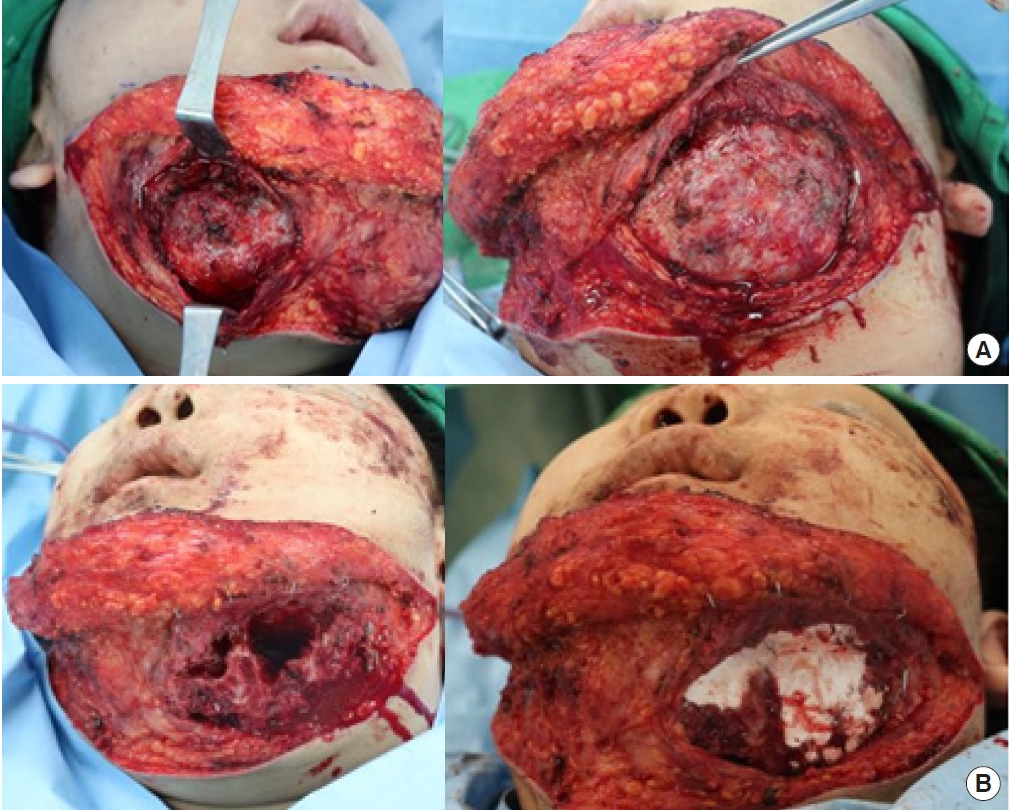
Photograph during surgery. (A) Enlarged bones are observed in both jaws. (B) Gross contouring of the bilateral body, angle, and ramus of the mandible was achieved using an osteotome, while delicate contouring was accomplished with a bone burr and curettage. Demineralized bone matrix was used to fill multiple locular bone defects that remained after contouring through osteotomy and bone burring.
A histologic examination of the mandible fragment obtained during surgery revealed numerous giant cells within a fibrous stroma, resembling a central giant cell granuloma (hematoxylin and eosin staining, × 100) (Fig. 4). Following the surgery, he was admitted to the intensive care unit and underwent an immediate tracheostomy. The tracheostomy was removed on postoperative day 2, and the patient was transferred to a general ward on postoperative day 3. Initially, the Barovac drained over 100 cc in the first 24 hours post-surgery, but the output decreased to 10 cc or less per day thereafter. The Barovac was removed, and all stitches were removed on postoperative day 6. The patient was discharged on postoperative day 8 without experiencing any specific acute complications.
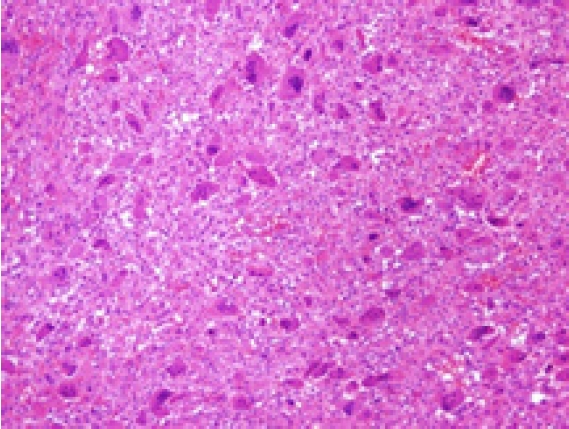
Microscopic photographs of the surgically obtained specimen. A histologic examination of the mandible fragment obtained during surgery revealed numerous giant cells within a fibrous stroma, resembling a central giant cell granuloma (hematoxylin and eosin staining, ×100).
We are conducting regular outpatient department follow-up visits to monitor for any aggravation of cherubism and to manage the scarring at the incision site. During the 8-month postoperative follow-up period, there were no complications, such as infection or hematoma, and the facial contour remained stable with no signs of cherubism progression (Fig. 5). Additionally, the patient expressed satisfaction with the cosmetic outcome.
LITERATURE REVIEW
Cherubism, first described in 1933 by Jones, is classified as a rare disease by the National Institutes of Health. Its prevalence is unknown, with approximately 300 cases reported in the medical literature [2]. According to the World Health Organization classification, cherubism falls under the histological category of osseous lesions. Unlike central giant cell granuloma and giant cell tumor, which share similar histologic characteristics, cherubism is genetically transmitted and typically presents earlier, with extensive and bilateral jaw involvement [2]. This familial disorder exhibits an autosomal dominant inheritance pattern and is linked to mutations in the SH3BP2 gene on chromosome 4p16.3. It shows variable penetrance and expressivity, with 100% in males and 50%–70% in females [1]. The incidence is higher in men than in women, with a ratio of 2:1 [5]. Radiographically, cherubism can be detected between the ages of 18 months and 2 years. It tends to progress slowly during adolescence, with spontaneous regression typically beginning after puberty and continuing into the twenties. Due to the naturally fuller faces of children, parents may not notice mandibular expansion until it is significantly advanced [5].
Typically, bilateral, multilocular, and radiolucent areas are involved in the mandible, with the ramus and angle being primarily affected [2]. The coronoid process is frequently involved, whereas the condyle is rarely affected. Lesions in the mandible tend to be symmetrical, whereas those in the maxilla are usually asymmetrical. In advanced stages, maxillary lesions may invade the orbital region, resulting in an upward tilting of the eyeball. Other cranial bones are generally unaffected [2]. In some instances, the second and third molars may be congenitally missing, and deciduous teeth may be lost prematurely. The positioning of the permanent teeth can be altered by jaw lesions, leading to malocclusion. Imaging studies typically reveal expansive bone remodeling and cortical thinning with a trabecular pattern and multilocular radiolucent areas [5]. Histologically, the lesion is a non-neoplastic fibrotic condition characterized by numerous multinucleated giant cells and, occasionally, cysts [7]. Additionally, there is often an increase in newly formed bone matrix and osteoid at the periphery.
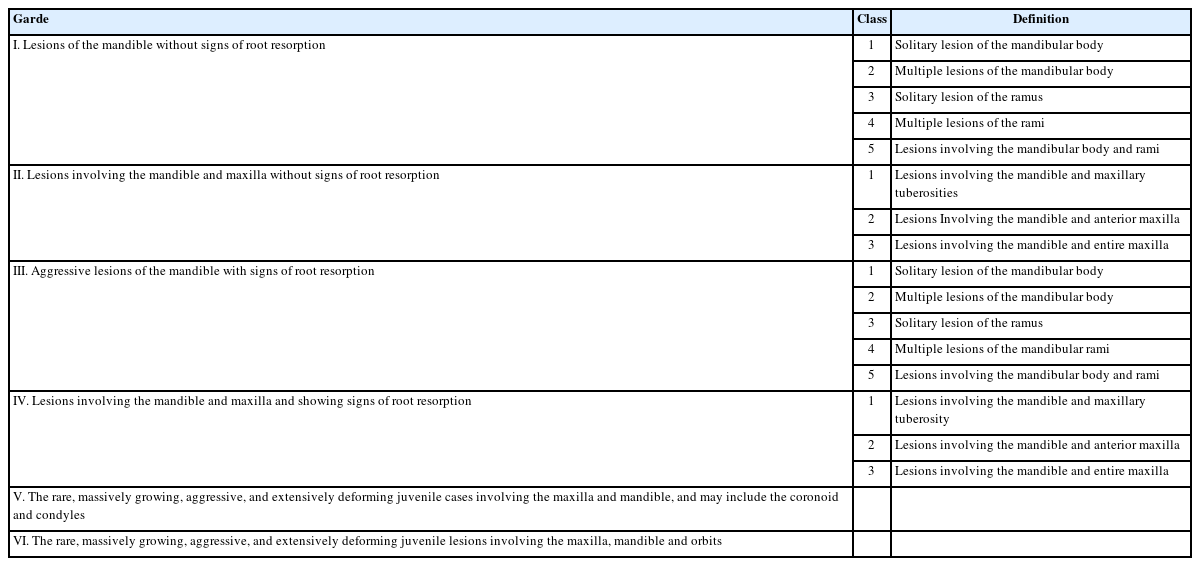
Diagnosis is primarily based on a combination of typical clinical presentation, imaging studies, and histologic examination. Additionally, if necessary, the identification of a pathogenic variant of the SH3BP2 gene through molecular genetic testing is recommended [2]. While some experts argue that a tissue biopsy is sufficient to confirm a diagnosis, others emphasize that the histologic findings of cherubism are similar to those of other jaw-invading tumors. Given the distinct treatment approaches, exercising caution is crucial when relying solely on histologic findings for diagnosis [8]. Raposo-Amaral synthesized the classifications of Motamedi (1998) to grade cherubism, taking into account orbital involvement and dividing it into six grades. According to this classification, the patient corresponds to grade VI (Table 1).
The widely accepted treatment for cherubism is observation, as it often resolves spontaneously [9]. Some studies suggest that the increased activity of osteoclasts typically normalizes at puberty due to the increased synthesis of sex steroid hormones [10]. However, surgical intervention may be necessary before puberty, which could include the extraction of teeth from areas of fibrous changes, osteoplasty of the jaws, and curettage of pathological lesions [2,11]. Larger clinical studies indicate that curettage and more conservative surgical measures are the predominant treatments [4]. Nevertheless, the removal of extensively distended bone is not recommended to avoid the risk of pathologic fracture [7]. Recent studies have advocated for early surgical intervention, taking into account the impact of cosmetic concerns on mental development and acknowledging that some cases may not regress by adulthood [9]. In some patients, pathologic tissue can be removed via liposuction [12]. Consequently, there is debate regarding the indications for surgical intervention in cherubism, as well as the optimal timing and surgical technique.
Some studies have suggested the use of medications such as calcitonin, immunomodulators, and anti-resorptive agents as potential cures. Calcitonin, in particular, has been used experimentally to treat cherubism, showing an ability to inhibit bone resorption in in vivo experiments [13]. However, caution is advised in using calcitonin for rapidly growing lesions, as its impact on giant cell granulomas may not be apparent for an extended period, potentially up to 18 months [14]. Although several cytokines have been implicated in the pathophysiology of the disease, and biomarkers like tumor necrosis factor-α (TNF-α) and nuclear factor of activated T-cells, cytoplasmic 1 (NFATc1) are believed to play a role, their effectiveness has not been conclusively proven in studies.
DISCUSSION
Cherubism is a rare fibro-osseous condition characterized by bilateral expansion of the mandible and maxilla. Due to its rarity, treatment guidelines for cherubism have not been clearly established. Despite its low incidence, some patients experience physical and psychological discomfort as a result of the condition.
In this case, surgical treatment for an enlarged mandible involved contour resection with osteotomy, bone burring, and curettage. To address the multiple locular defects remaining after contouring, contour filling was performed using demineralized bone matrix in a patient with cherubism. The patient’s symptoms had begun at the age of 7 and persisted into early adulthood without spontaneous resolution. Histologic analysis of the surgical specimen revealed giant cells within a fibrous stroma, findings that are consistent with the characteristic histology of cherubism [7]. During the 8-month postoperative follow-up, there was no progression of cherubism in the operated mandible, and no other unusual complications were noted. The patient reported satisfaction with the improved appearance and cosmetic outcome. Future surgical plans include bone resection of the bilateral orbital floor and contouring of the bilateral maxilla to correct orbital dystopia. This will not be a single procedure but will likely involve multiple surgeries, with the ultimate goal of establishing a framework for dentition using a bone flap. To achieve this, we are actively collaborating with dentists, otolaryngologists, and ophthalmologists.
Cherubism is not only an extremely rare condition globally, but also one with few reported cases in Korea. Furthermore, the guidelines and timing for the treatment of cherubism are not clearly established. We hope that the findings from this case study, which focuses on the treatment methods and outcomes of cherubism persisting into early adulthood, will contribute to the development of effective treatment approaches for this condition.
Notes
Conflict of interest
No potential conflict of interest relevant to this article was reported.
Funding
None.
Ethical approval
The report was approved by the Institutional Review Board of Ilsan Paik Hospital (IRB No. ISPAIK 2023-10-027).
Patient consent
The patient provided written informed consent for the publication and use of his images.
Author contributions
Conceptualization: Youngwoong Choi. Writing - original draft: Choong Hyeon Kim. Writing - review & editing: Choong Hyeon Kim, Jeong Min Ji, Ki Pyo Sung, Youngwoong Choi. Resources: Choong Hyeon Kim, Ki Pyo Sung, Youngwoong Choi. Supervision: Youngwoong Choi.