The branching patterns and termination points of the facial artery: a cadaveric anatomical study
Article information
Abstract
Background
The facial artery is an important blood vessel responsible for supplying the anterior face. Understanding the branching patterns of the facial artery plays a crucial role in various medical specialties such as plastic surgery, dermatology, and oncology. This knowledge contributes to improving the success rate of facial reconstruction and aesthetic procedures. However, debate continues regarding the classification of facial artery branching patterns in the existing literature.
Methods
We conducted a comprehensive anatomical study, in which we dissected 102 facial arteries from 52 embalmed and formaldehyde-fixed Vietnamese cadavers at the Anatomy Department, University of Medicine and Pharmacy, Ho Chi Minh City, Vietnam.
Results
Our investigation revealed eight distinct termination points and identified 35 combinations of branching patterns, including seven arterial branching patterns. These termination points included the inferior labial artery, superior labial artery, inferior alar artery, lateral nasal artery, angular artery typical, angular artery running along the lower border of the orbicularis oculi muscle, forehead branch, duplex, and short course (hypoplastic). Notably, the branching patterns of the facial artery displayed marked asymmetry between the left and right sides within the same cadaver.
Conclusion
The considerable variation observed in the branching pattern and termination points of the facial artery makes it challenging to establish a definitive classification system for this vessel. Therefore, it is imperative to develop an anatomical map summarizing the major measurements and geometric features of the facial artery. Surgeons and medical professionals involved in facial surgery and procedures must consider the detailed anatomy and relative positioning of the facial artery to minimize the risk of unexpected complications.
INTRODUCTION
The facial artery, which originates from the external carotid artery, plays a critical role in supplying the anterior face with the majority of its blood supply. It starts at the border of the lip, crosses the jaw, and ascends between the nostrils and the cheek, ultimately reaching the submandibular gland [1]. Although the facial artery has been the subject of numerous studies, there is still ongoing debate in the literature about its classification, branching structure, and termination points. Various authors have proposed classifications for the branching patterns of the facial artery across the face, but a consensus has yet to be established [2-5].
Extensive anatomical investigations of dissected cadavers have provided valuable insights into the facial artery [2-14]. Previous research has identified the angular, superior, and inferior labial arteries, as well as the lateral nasal arteries (LNAs) or alar arteries, named for the anatomical regions they supply. However, the complexity of the branching patterns and the termination point of the facial artery has been obscured by the use of different terminologies in various studies.
Several studies have attempted to categorize the facial artery based on its distribution. Pinar et al. [15], Loukas et al. [10], and Koziej et al. [7] identified five distinct types of facial artery distribution, while Yang et al. [16], Dickson et al. [2], and Niemann et al. [12] reported six types. Furukawa et al. [4] described four types. The identification of the ultimate branch of the facial artery is still a subject of debate in the field. In this study, we used the terminology from Terminologia Anatomica (2020), abbreviated as TA98, for the well-known tributaries of the facial artery: the inferior labial artery (ILA; TA2 code: A12.2.05.025), the superior labial artery (SLA; TA2 code: A12.2.05.026), and the lateral nasal branch (TA2 code: A12.2.05.028). Although the branch that supplies the ala of the nose is not listed in TA2, it is commonly referred to as the inferior alar branch.
Recent anatomical investigations have shed light on the branching patterns of the ILA. Two distinct patterns have been observed. The first pattern follows the vermilion border of the lower lip and emerges from the facial artery at the cheilion (mouth corner). The second pattern, referred to as the horizontal labiomental artery (hLMA), descends along the labiomental crease and passes beneath the cheilion. Al-Hoqail and Meguid [1] and Kawai et al. [17] have noted that the submental artery can adopt the first pattern, giving rise to the vertical labiomental arteries, or it can divide into multiple vertical branches of the hLMA and anastomose with the ILA. The terminal tributary of the facial artery that enters the angular region is known as the angular artery (AA; TA98 code: A12.2.05.029). The AA can take two courses. The typical course runs along the side of the nose, while the AAOOc runs along the lower border of the orbicularis oculi muscle (OOc). Although the facial artery usually follows the first pattern, there are instances where it follows an atypical path along the lower border of the OOc, referred to as the zygomatic branch [15], infraorbital trunk [8], dominant lateral branch [4], or detoured branch [8]. The objective of this study was to conduct a comprehensive and detailed analysis of the branching structure and the termination points of the facial artery throughout the face.
METHODS
Specimen collection and preparation
This cross-sectional study was conducted in the Anatomy Department of the University of Medicine and Pharmacy at Ho Chi Minh City, Vietnam, from March to December 2021. A total of 52 adult Vietnamese cadavers, which had been embalmed and fixed with formaldehyde, were selected for the dissection of the facial artery. The cadavers were sourced from various individuals who had donated their bodies for medical education and research purposes.
Dissection procedures
A team of experienced anatomists and medical professionals conducted the dissections. Each cadaver underwent a thorough examination before dissection to ensure there were no craniofacial anomalies or pathologies that might compromise the integrity of the facial arteries. The dissection protocol adhered to the standardized anatomical guidelines detailed in Cunningham’s Manual of Practical Anatomy [18]. The dissections took place under controlled laboratory conditions, with the team using appropriate personal protective equipment and surgical instruments.
To access the facial arteries, a midline incision was made along the neck and face. The skin, platysma, and superficial fascia covering the carotid triangle on both sides were meticulously reflected laterally. After reflecting the deep cervical fascia, the boundaries of the sternocleidomastoid muscles and the superior belly of the omohyoid were identified. Careful dissection techniques were employed to avoid any damage to the surrounding structures.
Next, the submandibular gland was mobilized by delineating the boundaries of the posterior bellies of the digastric and stylohyoid muscles. Upon opening the carotid sheath within the carotid triangle, the external carotid artery and its branches were identified. The external carotid artery in the neck features three primary branches, with the facial artery being the third. This approach improved visualization and access to the carotid sheath, enabling the clear identification of the external carotid artery and its branches. The facial artery, as the third branch of the external carotid artery in the neck, was carefully traced and dissected.
Throughout the dissection process, a × 2.5 magnification loupe was utilized to enhance precision and accuracy. The branching patterns and termination points of the facial artery within the face were meticulously observed and documented. Dissections were performed on a total of 102 hemifaces, obtained from 52 cadavers.
Data collection and analysis
Detailed notes were taken and anatomical drawings were made during the dissection process to document the observed branching patterns and termination points of the facial artery. The data collected were then organized and analyzed to identify common patterns and variations. Statistical analyses, including frequency distributions and descriptive statistics, were used to summarize the findings. The results were presented in tables and accompanied by anatomical illustrations to offer a comprehensive visual representation of the branching patterns and termination points of the facial artery.
Quality control measures
To ensure the accuracy and reliability of our findings, we implemented quality control measures throughout the dissection process. The dissection team engaged in regular discussions and consultations to address any discrepancies or uncertainties encountered. Additionally, cross-validation of observed patterns and measurements was performed by multiple experienced anatomists to enhance the validity of the data.
RESULTS
The study included 52 adult Vietnamese cadavers, with an average age at death of 74.31 years, ranging from 32 to 100 years. Among these cadavers, 17 were female and 35 were male. The researchers dissected a total of 102 facial arteries from the cadavers. Of the 52 cadavers, 50 were used to obtain the 102 facial arteries, with an equal number of 51 arteries dissected from both the left and right sides. Additionally, one artery from each side was included despite tissue injury. The majority of the facial arteries, 95%, originated directly from the external carotid artery. In contrast, 6% arose from the linguofacial trunk, and 1% from the thyrolingual trunk.
The 102 evaluated facial arteries exhibited a range of branches by the following frequencies: one branch was observed in eight cases (7.84%), two branches in 13 cases (11.75%), three branches in 28 cases (27.45%), four branches in 33 cases (32.35%), five branches in 18 cases (17.65%), six branches in one case (0.98%).
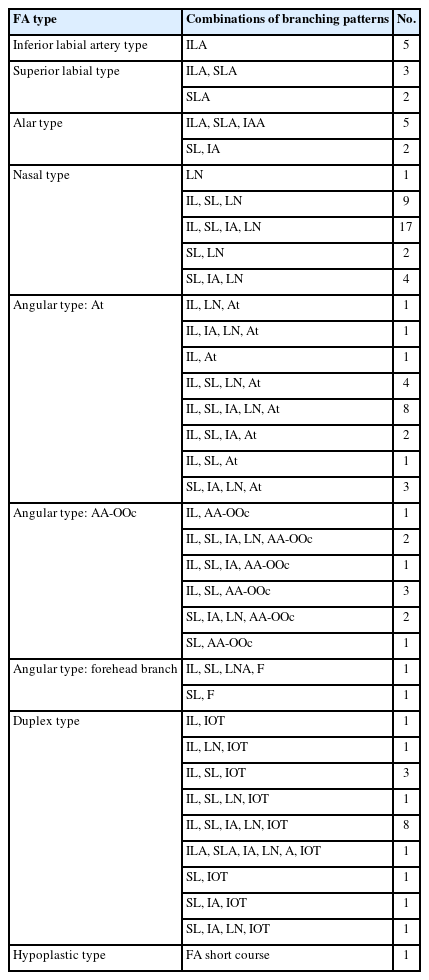
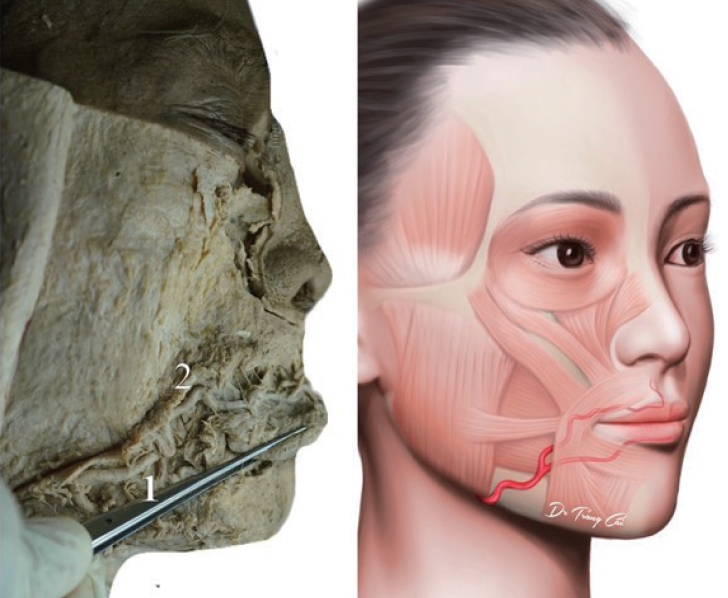
The facial artery has eight types of branches (ILA, SLA, inferior alar artery [IAA], LNA, AA typical, AA-OOc, forehead branch, and duplex) in 35 combinations (Table 1). Importantly, the branching patterns and termination sites were found to be asymmetrical between the left and right sides. Additionally, these facial arteries provided arterial blood supply to the respective opposing sides of the face.
Among eight types of branches, the SLA was the most prevalent branch, accounting for 89 specimens (87.25%), followed by the ILA 80 specimens (78.43%), LNA 67 specimens (64.71%), 59 specimens IAA (57.84%), AA typical 22 specimens (21.57%), AA-OOc 10 specimens (9.80%), forehead branch two specimens (1.96%), and duplex 18 specimens (17.65%). In one specimen (0.98%), the facial artery exhibited a brief course in the inferior labial area. On the other hand, one specimen had AA and duplex together (Table 1).
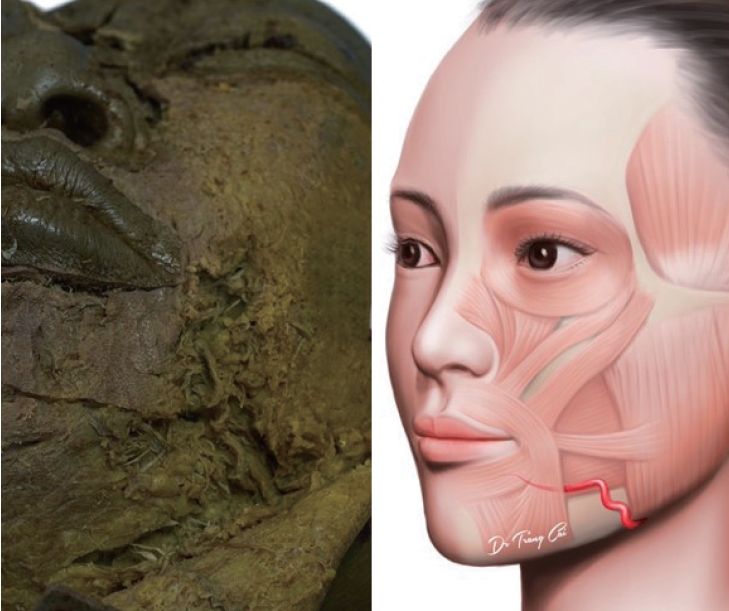
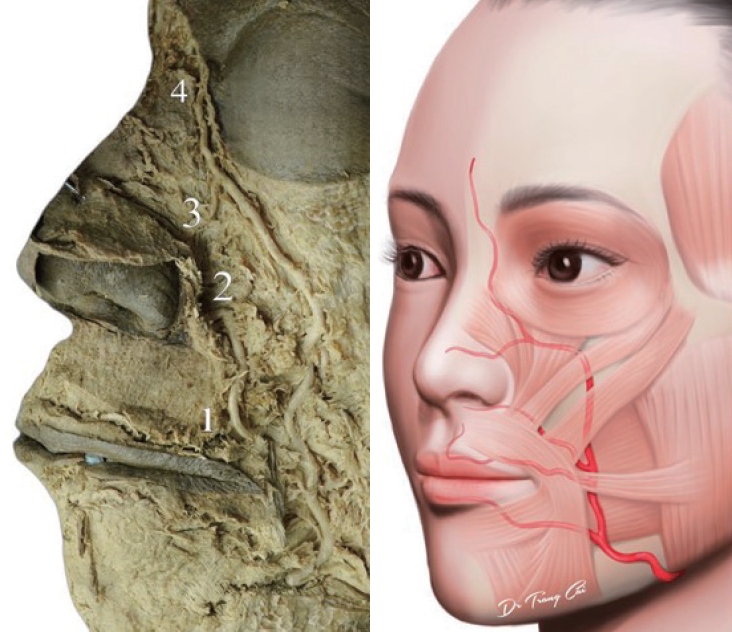
Of the 80 ILAs observed, nine displayed the first typical ILA pattern (Fig. 1), while 71 displayed the second pattern known as hLMA or ILA with a hLMA pattern (Figs. 2-7).
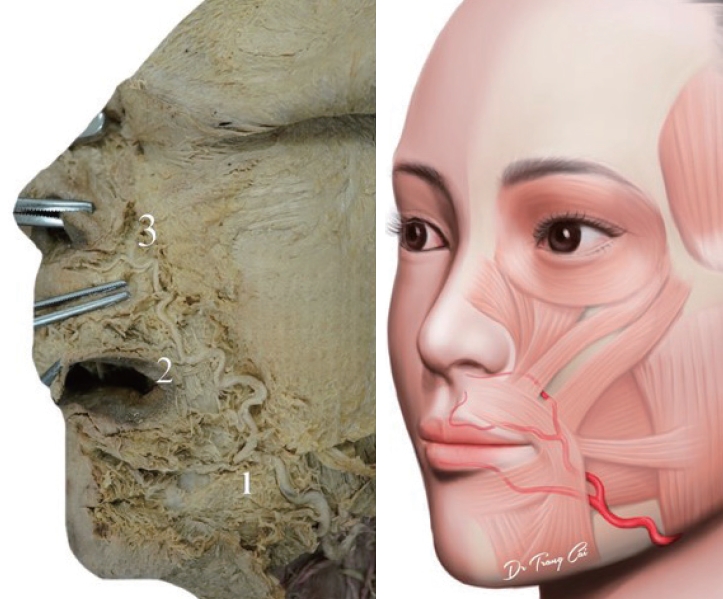
Facial artery, duplex type. (1) The inferior labial artery (ILA), typical ILA. (2) The superior labial artery. (3) The inferior alar artery (IAA), IAA from facial artery. (4) The lateral nasal artery. (5) The infraorbital trunk.

Facial artery, inferior labial type. (1) The inferior labial artery (ILA) horizontal labiomental artery (hLMA) or ILA with a hLMA pattern. (2) The transverse facial artery.
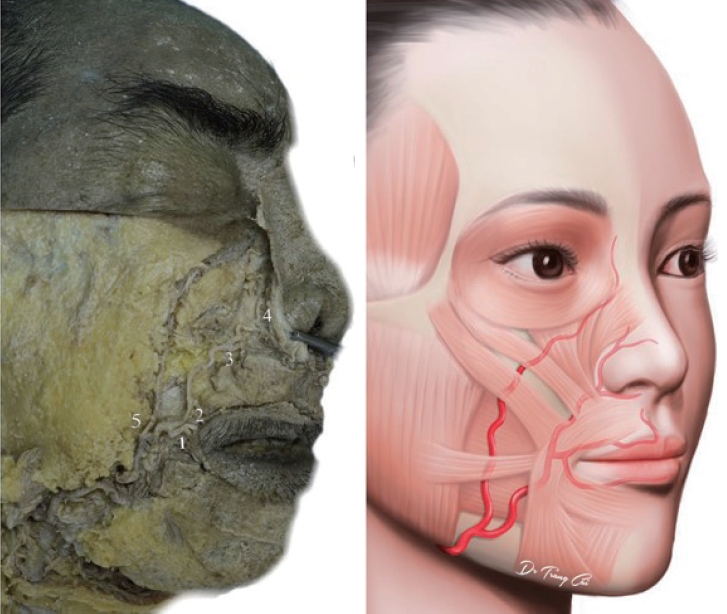
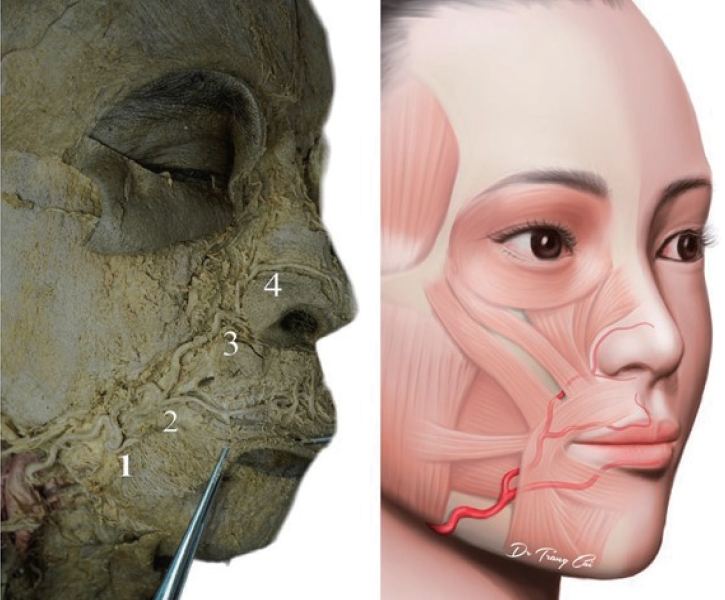
Facial artery, superior labial type. (1) The inferior labial artery (ILA) horizontal labiomental artery (hLMA) or ILA with a hLMA pattern. (2) The superior labial artery.
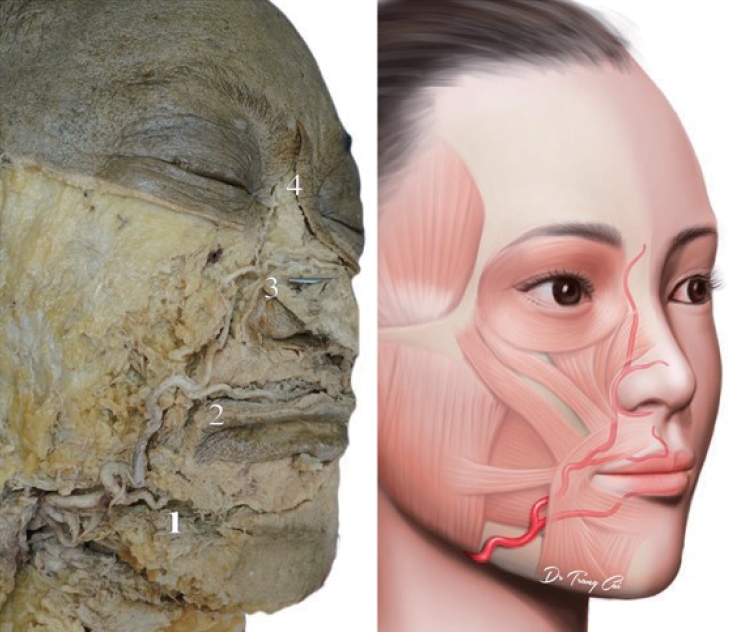
Facial artery, alar type. (1) The inferior labial artery (ILA) horizontal labiomental artery (hLMA) or ILA with a hLMA pattern. (2) The superior labial artery. (3) The inferior alar artery (IAA), IAA from facial artery.
Facial artery, nasal type. (1) The inferior labial artery (ILA) horizontal labiomental artery (hLMA) or ILA with a hLMA pattern. (2) The superior labial artery. (3) The inferior alar artery (IAA), IAA from facial artery. (4) The lateral nasal artery.
Facial artery, angular typical type. (1) The inferior labial artery (ILA) horizontal labiomental artery (hLMA) or ILA with a hLMA pattern. (2) The superior labial artery. (3) The lateral nasal artery. (4) The angular artery typical type.
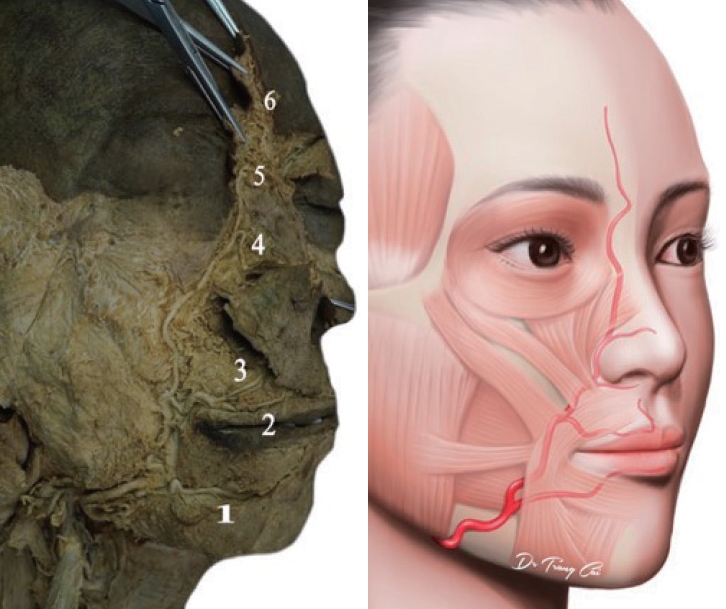
Facial artery, angular type with forehead branch. (1) The inferior labial artery (ILA) horizontal labiomental artery (hLMA) or ILA with a hLMA pattern. (2) The superior labial artery (SLA). (3) The inferior alar artery (IAA), IAA from SLA. (4) The lateral nasal artery. (5) The angular artery. (6) Forehead branch.
Furthermore, out of 59 IAAs from facial artery (Figs. 1, 4, 5, 8), there were 13 IAAs not a branch of the facial artery. These IAAs originated from the SLA in six cases (Fig. 7), the contralateral SLA in four cases, the contralateral LNA in two cases, and the infraorbital artery in one case.
Figs. 1-9 show the branching patterns of 102 facial arteries according to their terminations. Eight distinct termination points are ILA, SLA, IAA, LNA, AA, forehead branch, duplex and under the inferior labial area (hypoplastic type). The results showed that the facial artery terminated as ILA in five cases (4.90%) in Fig. 2, as SLA in five cases (4.90%) in Fig. 3, as IAA in seven cases (6.86%) in Fig. 4, as LNA in 33 cases (32.35%) in Fig. 5, as AA in 31 cases (30.39%) in Figs. 6 and 8, as forehead branch in two cases (1.96%) in Fig. 7. Notably, in the duplex of 18 cases (17.65%) in Fig. 1, a prominent lateral angular branch traveled down the nasojugal groove, along the lower border of the OOc before terminating at the nasion. The duplex facial artery type exhibited nine combination patterns (Table 1). In one instance, the facial artery terminated under the inferior labial area after a brief course (Fig. 9).
Facial artery, angular AA-OOc type. (1) The superior labial artery. (2) The inferior alar artery (IAA), IAA from facial artery. (3) The lateral nasal artery. (4) The angular artery along the lower border of the orbicularis oculi muscle type (AA-OOc type).
Furthermore, 48 out of 102 cases (47.05%) had an ophthalmic artery with a dorsal nasal artery. Among these cases, there were three instances of the ILA type, two instances of the SLA type, 37 instances of the nasal angular type, and eight instances of the duplex type. Additionally, in three out of five cases, the transverse facial artery (Fig. 2), which is a kind of ILA, supplied blood to the lip and nose. In the case of the hypoplastic facial artery, the contralateral facial artery supplied the full remaining course.
DISCUSSION
The findings of our study lead to several significant conclusions. First, we have identified eight distinct termination points on the superior/distal aspect of the facial artery. Second, Table 1 provides a comprehensive overview of the 35 different branching patterns observed in the facial artery. Third, it is important to note the asymmetrical characteristics between the left and right sides of the face. Fourth, in rare cases, the facial artery may cross the midline to supply arterial blood to the opposite side of the face. Additionally, our study reveals discrepancies between our findings and those from previous studies regarding the branching patterns and termination points of the facial arteries. These differences raise questions about the reliability and utility of existing categorization schemes.
In our investigation, we observed a range of 1 to 6 visualized branches in the assessed frontal arteries, with the percentages of occurrence ranging from 0.98% for one branch to 31.37% for four branches. When compared with other studies, there are noticeable variations in the number of branches identified. For instance, Koziej [7] utilized computed tomographic angiography to analyze 255 facial arteries and found the following distribution: 35 cases (13.7%) had one branch, eight cases (3.1%) had five branches, 45 cases (17.6%) had four branches, 88 cases (34.5%) had three branches, 72 cases (28.2%) had two branches, and seven cases (2.7%) exhibited the hypoplastic type. An anatomical cadaver study of Kulkarni and Geetha [19] reported different branch counts: six branches in two cases, seven branches in 18 cases, eight branches in 43 cases, nine branches in 36 cases, and 10 branches in one case. These discrepancies underscore the necessity for additional research to achieve a consistent understanding of the branching patterns of the facial artery.
The reported prevalence of certain branch of FA, such as the AA, SLA, and ILA, also varies across studies [6,8] from 32.5% to 73.5% for the AA, from 77.5% to 98.0% for the SLA, and from 57.5% to 100% for the ILA. Our study yielded prevalence rates of 33.33%, 87.25%, and 78.43% for these arteries, respectively.
Recent anatomical investigations have shed light on the branching patterns of the ILA. Two distinct patterns have been observed [8]. The first pattern follows the vermilion border of the lower lip and emerges from the facial artery at the cheilion (mouth corner). The second pattern, referred to as the hLMA, descends along the labiomental crease and passes beneath the cheilion. Kawai et al. [17] and Al-Hoqail and Abdel Meguid [1] have noted that the submental artery can adopt the first pattern, giving rise to the vertical labiomental arteries, or it can divide into multiple vertical branches of the hLMA and anastomose with the ILA. The use of different terminologies and classifications by researchers may contribute to these discrepancies. Furthermore, there is no consensus on which branch of the facial artery should be considered as the ultimate termination point. While the AA is commonly regarded as the final branch, it can also arise from the ophthalmic or infraorbital arteries.
Regarding the termination vessels, studies have reported varying prevalence rates for different types, such as from 0% to 80% for an IAA, 0% to 15% for a LNA or AA, 0% to 95.16% for a duplex artery, and 0% to 8.33% for a hypoplastic facial [6-8]. In our study, out of 102 assessed facial arteries, the termination was AA/F in 33 cases (32.35%), LNA in 33 cases (32.35%), IAA in seven cases, SLA in five cases, and ILA in five cases. Furthermore, we observed nine combination patterns with a duplex artery in 18 facial arteries (17.65%). These findings provide the most recent information about facial artery termination. In our study, the traditional definition of the AA as the facial artery’s terminal tributary only had a success rate of 32.35%. Therefore, our results suggest that the LNA and AA are the primary terminations of the facial artery, which is consistent with findings from other studies (Table 2). The termination point of the facial artery exhibited remarkable consistency in its characteristics, suggesting its potential utility in categorizing the branching pattern of the facial arteries. In our investigation, we have identified seven distinct types as follows: (1) angular type: facial artery terminates at the AA or forehead branch; (2) nasal type: facial artery terminates at the LNA; (3) alar type: facial artery terminates at the IAA; (4) superior labial type: facial artery terminates at the SLA; (5) inferior labial type: facial artery terminates at the ILA; (6) duplex type: facial artery terminates as a duplex artery with the infraorbital trunk; and (7) hypoplastic type: hypoplastic facial artery.
In conclusion, eight termination points of the facial artery were observed, with 35 different branching patterns that showed asymmetries between the left and right sides. The usual description of the AA as the facial artery’s terminal tributary was accurate in only 32.35% of cases. The duplex type was found in 18 facial arteries (17.65%). Differences according to the branching pattern and termination points of the facial artery should be considered to reduce complications during while performing head and neck surgery, facial plastic surgery, and facial aesthetic procedures.
Notes
Conflict of interest
No potential conflict of interest relevant to this article was reported.
Funding
This study was supported by the University of Medicine and Pharmacy, Ho Chi Minh City, Vietnam.
Ethical approval
This study was approved by the University of Medicine and Pharmacy at Ho Chi Minh City 2 (No. IRB-VN01002/IRB00010293/FWA00023448).
Author contributions
Conceptualization; Data curation; Formal analysis; Methodology; Project administration: Vu Hoang Nguyen, Trang Huu Ngoc Thao Cai, Tuan Anh Nguyen, Lin Cheng-Kuan. Visualization: Vu Hoang Nguyen, Trang Huu Ngoc Thao Cai. Writing - original draft: Trang Huu Ngoc Thao Cai. Writing - review & editing: Trang Huu Ngoc Thao Cai, Vu Hoang Nguyen, Tuan Anh Nguyen, Lin Cheng-Kuan. Investigation: Vu Hoang Nguyen, Trang Huu Ngoc Thao Cai, Tuan Anh Nguyen, Lin Cheng- Kuan. Resources: Vu Hoang Nguyen, Trang Huu Ngoc Thao Cai. Software: Trang Huu Ngoc Thao Cai, Lin Cheng-Kuan. Supervision; Validation: Vu Hoang Nguyen, Trang Huu Ngoc Thao Cai, Tuan Anh Nguyen, Lin Cheng-Kuan.
Abbreviations
AA
angular artery
hLMA
horizontal labiomental artery
IAA
inferior alar artery
ILA
inferior labial artery
LNA
lateral nasal artery
OOc
orbicularis oculi muscle
SLA
superior labial artery