Unexpected postoperative atlantoaxial rotatory subluxation after excision of melanocytic nevi of the head and neck in older children: two case reports and literature review
Article information
Abstract
Postoperative atlantoaxial rotatory subluxation (AARS) is a rare complication that develops almost exclusively in children following oropharyngeal and otologic surgeries, proposing that oropharyngeal inflammatory responses and excessive head rotation are responsible factors. However, there have been no reports of AARS after excision of a nevus on the head and neck. Here, we present two cases of AARS following limited head rotation during simple nevus excision. Patient 1, a 9-year-old girl, complained of neck pain and limited range of motion after excision of the nevus on the neck. After 2 months, computed tomography and magnetic resonance imaging finally revealed AARS with a ruptured transverse atlantal ligament. A month of halo traction was required for the treatment. Patient 2, an 11-year-old girl, presented with immediate pain and limited neck extension after tissue expander insertion under the upper chest and excision of the nevus on her left cheek. The diagnosis was promptly made using cervical spine radiography. A cervical collar was applied for 1 month. Both patients recovered without any complications after treatment. This report highlights the importance of suspicion for AARS after surgery regardless of surgical duration or amount of head rotation.
INTRODUCTION
Postoperative atlantoaxial rotatory subluxation (AARS) is a rare complication that occurs mostly in children, manifesting with a wide range of symptoms, from minor neck discomfort to severe neurological deficits. There have been several case reports of AARS after surgery of the oropharynx [1-3] or the ear [4,5]. AARS after oropharyngeal surgery has been described as a consequence of oropharyngeal inflammatory response combined with a common venous and lymphatic drainage system of the oropharynx and atlantoaxial joint [6]. AARS after ear surgery has been considered a result of excessive head rotation during the surgery. However, to the best of our knowledge, there have been no reports of AARS developing after non-otolaryngologic surgery without evidence of inflammation or other predisposing factors. Here, we present two patients, aged 9- and 11-year-old, who developed postoperative AARS after nevus excision on their head and neck, performed with a limited range of head rotation over a short period.
CASE REPORT
Case 1
Patient 1 was a previously healthy 9-year-old girl (139.5 cm, 33.7 kg) whose growth was within the normal range. She had a 3× 2.5 cm sized melanocytic nevus on her left neck and underwent partial excision under general anesthesia. During surgery, the head was rotated to the right at an angle of 60° for 25 minutes. There were no abnormal events during or after awakening from general anesthesia. The patient complained of postoperative neck pain and limited cervical range of motion (ROM) immediately after the surgery. Since the surgery was simple and short, the surgeon believed that the pain was mainly psychological and provided reassurance. As the neck pain and ROM limitation persisted for 2 months after surgery, a consultation was made to the rehabilitation medicine department for physical therapy. The atlantodental interval (ADI) could not be measured on plain radiographs in a fully flexed position because of the restricted neck motion. For the same reason, dynamic computed tomography (CT) scan could not be performed. Instead, static CT and magnetic resonance imaging (MRI) clearly revealed AARS with a ruptured transverse atlantal ligament (Fig. 1). After 1 month of halo traction, the follow-up CT scan showed almost resolved AARS (Fig. 2). Post-reduction immobilization was performed using a halo vest for 4 months. The pain and neck ROM recovered completely without any complications.
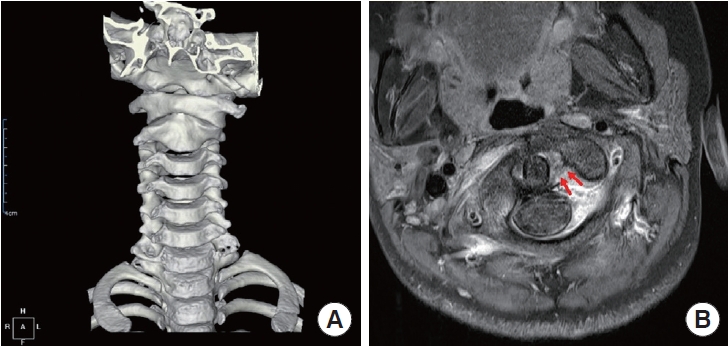
A 9-year-old girl with persistent neck pain and limited range of motion after excision of a nevus on the neck. (A) Static computed tomography revealed atlantoaxial rotatory subluxation with counterclockwise rotation. (B) Cervical magnetic resonance imaging confirmed atlantoaxial rotatory subluxation with a ruptured transverse atlantal ligament (arrows).
Case 2
Patient 2 was a previously healthy 11-year-old girl (138 cm, 29 kg) whose growth was within the normal range. She had a giant hairy nevus on her chest and neck, and multiple nevi on her left cheek. She had already undergone eight times of tissue expander insertions and removals without complications. At this time, she underwent another tissue expander insertion at the neck, as well as excision of the nevus on her left cheek. The head was rotated to the right for approximately 20 minutes during excision of the nevus. The rotation angle was maintained under 60º. The total surgical time was 2 hours. One day after the surgery, the patient was unable to extend her neck due to pain. Cervical spine radiography revealed an increased ADI of 5.30 mm, which indicated AARS accompanying spondylolisthesis at the C3-C5 level (Fig. 3A). A prompt consultation was made with the orthopedic department, and a Philadelphia cervical collar was applied for 1 month. Diagnosis was confirmed solely with plain radiography, clinical symptoms and history. Dynamic CT scans or MRI were not performed, as they were deemed unnecessary procedures with poor cost-effectiveness. The patient showed full recovery of the cervical ROM without pain 1 week after collar application. After a month of cervical immobilization using a cervical collar, ADI was reduced to 3.21 mm, which was the normal range (Fig. 3B). No further treatment was required.
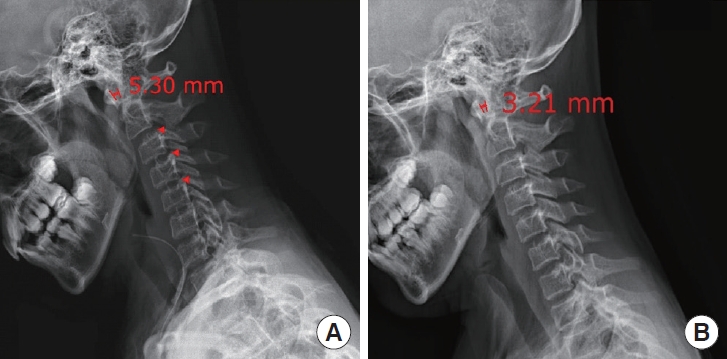
An 11-year-old girl with immediate pain and limited neck extension after tissue expander insertion under the upper chest and excision of a nevus on her left cheek. (A) Initial cervical spine radiograph revealed an increased atlantodental interval of 5.30 mm which indicated atlantoaxial rotatory subluxation accompanying spondylolisthesis in C3-C5 levels (arrowheads). (B) After 1 month of immobilization using a cervical collar, atlantodental interval was reduced to 3.21 mm, which was normal range.
LITERATURE REVIEW
AARS is an uncommon condition with several etiologies, including congenital, traumatic, inflammatory, iatrogenic (postoperative), and often multifactorial [7,8]. Postoperative AARS itself appears to be a condition of heterogeneous etiology. Early cases of postoperative AARS were primarily reported after oropharyngeal surgery, including pharyngoplasty or tonsillectomy. Their pathogenesis was described by the hematogenous spread of inflammation from the pharynx to the cervical spine [1,3,6,9]. Then several cases of AARS after otologic surgery were reported, which could not be explained by the inflammatory cause [4,6,10]. The cases were almost exclusively reported in children, whose paraspinal musculature is more immature, the spinal ligaments are more lax, and the facets are shallower and more horizontally oriented, which makes it more unstable than those of the adult spine [11-14]. Previous studies have concluded that excessive passive rotation of immature pediatric cervical spine under decreased muscle tone during general anesthesia may cause the postoperative AARS [4,10].
Diagnosing AARS involves a comprehensive approach including plain cervical radiography, dynamic CT, MRI, clinical symptoms and signs, and medical history [15]. The ADI, measured from plain radiographs, typically does not exceed 3 mm in adults and 5 mm in children [16,17]. An ADI is greater than 5 mm in children strongly suggests disruption of the transverse atlantal ligament [18,19]. The open-mouth odontoid view may reveal features suggestive of AARS, such as the displacement of the odontoid process and asymmetry of the C1 lateral masses (wink sign) [20,21]. Dynamic CT scan of the three phases, neutral and bilateral maximal rotation, is the gold standard diagnostic modality with higher specificity, evaluating the C1-2 angles and resistance to normal motion [9,22,23]. Yet, its reliability and reproducibility in the acute phase remain controversial [24,25]. Some authors also questioned the cost-effectiveness of the routine use of dynamic CT scan, as acute symptoms usually resolved with simple cervical immobilization [26]. MRI can provide further information regarding soft tissue injury, such as disruption of the transverse atlantal ligament, bone or soft tissue infection, or spinal cord compression [27,28].
The treatment methods and prognosis of AARS depend on the timing of the diagnosis. Early detection leads to better outcomes with nonoperative management, whereas treatment delays exceeding 2–3 months may necessitate more aggressive intervention. Most acute cases (< 4 weeks) respond to analgesics and a soft cervical collar [29,30]. Still, up to 20% of cases can go chronic despite conservative treatment [29,31]. Persistent symptoms or treatment delays (> 4 weeks) make reduction challenging, requiring cervical traction and prolonged post-reduction immobilization [30]. AARS with symptoms persisting for > 3 months has a non-reducible rate of 50%, with a 50% risk of requiring surgical fusion [10,24].
DISCUSSION
Postoperative AARS, not involving a direct approach to the oropharynx, has predominantly been associated with otologic surgery requiring significant amount and duration of head rotation. However, our cases present a novel possibility for postoperative AARS following non-otolaryngologic surgery with modest head rotation. To the best of our knowledge, no such case has been reported previously.
Otologic surgeries associated with postoperative AARS required significant head rotation for at least 1 hour, with an average duration of 2.5 hours [4,6,10]. In contrast, our patients underwent modest head rotation for less than 30 minutes. Immaturity of the pediatric cervical spine may also play a key role in the development of AARS. However, AARS is less likely to occur in older school-aged children, such as our patients, presenting greater anatomical maturity compared to the younger population [14].
To explain the development of AARS despite old age and low-risk surgical procedure, we hypothesized that poor habitual neck posture could affect the cervical spine stability, thereby elevating the risk of injury. While no study has established the direct association between the AARS and habitual neck posture, forward head posture is well known to compromise cervical spine biomechanics and increase the risk of injury [32,33].
Both patients were girls in higher grades of elementary school, a phase marked by an expanding social environment and increased peer pressure. Preoperatively, they consistently exhibited forward head posture, slanting their necks forward to conceal their nevi. Notably, patient 2 had structural difficulties in neck extension because of the scar contracture from previous operations.
Pediatric patients often undergo surgical excision for nevi or tumors on their head and neck, not only because of malignancy concerns or functional deficits but also to improve cosmetically and socially unacceptable appearances [34-37]. These patients may adopt a forward head posture to hide visible lesions. According to our hypothesis, such patients may carry an increased risk of postoperative AARS due to the cervical instability resulting from poor habitual neck posture combined with moderate head rotation during general anesthesia. Thus, while preoperative radiographic screening for AARS lacks conclusive evidence [38], we suggest that pediatric patients with inappropriate cervical posture undergo preoperative plain cervical radiography. This can help assess preoperative cervical spine instability and guide careful management of neck rotation during surgery. Nonetheless, further prospective studies are essential to validate the presented hypothesis.
Our cases underscore the critical role of timely diagnosis in AARS prognosis. Patient 1’s delayed diagnosis led to extensive treatments and burdens, whereas immediate diagnosis for patient 2 resulted in swift recovery with minimal intervention. This highlights the need not only for prevention but also for early suspicion and diagnosis. Surgeons must be alert to possibility of AARS, ensuring timely radiologic studies and orthopedic consultations.
In conclusion, this study, unique in reporting postoperative AARS after modest head rotation in non-otolaryngologic surgery, highlights the importance of suspicion even in seemingly unlikely scenarios. Poor neck posture emerges as a potential risk factor, yet further investigations are needed to establish a definitive relationship.
Notes
Conflict of interest
No potential conflict of interest relevant to this article was reported.
Funding
None.
Ethical approval
The report was approved by the Institutional Review Board of Seoul National University Hospital (No. 2111-106-1272).
Patient consent
The patients provided written informed consent for the publication and use of their images.
Author contributions
Conceptualization: Byung Jun Kim. Data curation: Byung Jun Kim. Methodology: Jiwon Kang. Visualization: Jiwon Kang. Writing - original draft: Jiwon Kang. Writing - review & editing: Byung Jun Kim. Investigation: Jiwon Kang. Supervision: Byung Jun Kim.
Abbreviations
AARS
atlantoaxial rotatory subluxation
ADI
atlantodental interval
CT
computed tomography
MRI
magnetic resonance imaging
ROM
range of motion

