Kirschner Wire Fixation for the Treatment of Comminuted Zygomatic Fractures
Article information
Abstract
Background
The Kirschner wire (K-wire) technique allows stable fixation of bone fragments without periosteal dissection, which often lead to bone segment scattering and loss. The authors used the K-wire fixation to simplify the treatment of laborious comminuted zygomatic bone fracture and report outcomes following the operation.
Methods
A single-institution retrospective review was performed for all patients with comminuted zygomatic bone fractures between January 2010 and December 2013. In each patient, the zygoma was reduced and fixed with K-wire, which was drilled from the cheek bone and into the contralateral nasal cavity. For severely displaced fractures, the zygomaticofrontal suture was first fixated with a microplate and the K-wire was used to increase the stability of fixation. Each wire was removed approximately 4 weeks after surgery. Surgical outcomes were evaluated for malar eminence, cheek symmetry, Kwire site scar, and complications (based on a 4-point scale from 0 to 3, where 0 point is 'poor' and 3 points is 'excellent').
Results
The review identified 25 patients meeting inclusion criteria (21 men and 4 women). The mean age was 52 years (range, 15-73 years). The mean follow up duration was 6.2 months. The mean operation time was 21 minutes for K-wire alone (n=7) and 52 minutes for K-wire and plate fixation (n=18). Patients who had received K-wire only fixation had severe underlying diseases or accompanying injuries. The mean postoperative evaluation scores were 2.8 for malar contour and 2.7 for K-wire site scars. The mean patient satisfaction was 2.7. There was one case of inflammation due to the K-wire.
Conclusion
The use of K-wire technique was associated with high patient satisfaction in our review. K-wire fixation technique is useful in patient who require reduction of zygomatic bone fractures in a short operating time.
INTRODUCTION
The current standard correction of zygomatic fracture is based on wide exposure of all articulations, accurate reduction, and a rigid internal fixation with titanium or absorbable plates and screws [12]. When considering the treatment of bone fractures, an achievement of anatomical reposition and the application of a rigid internal fixation with more plates could be ideal. The number of plates required for fixation varies according to the degree of dislocation and type of fracture [23].
However, less invasive methods are becoming more popular for zygomatic fracture reduction. Closed reduction with Kirschner wire (K-wire) fixation is an alternative method in treating zygomatic fractures [45678]. It is simple, fast, and associated with decreased medical costs. Disadvantages of using K-wire fixation are unstable reduction, inaccurate fixation, and mal-union. Because of these disadvantages, the closed reduction with K-wire fixation is regarded as an outdated approach to zygomatic fracture and is used only occasionally for the simplest of zygomatic fracture by a small subset of craniofacial surgeons.
The K-wire allows fixation of the floating segments into the appropriate position without an injury to the periosteal. The authors have found that, because the closed approach spares the periosteum, the K-wire fixation is paradoxically effective for those who have comminuted fractures. In such patients, open reduction and rigid internal fixation of all bony fragments can be tedious. A wide dissection of the periosteum could scatter the small bone segments and also result in an impairment of the blood supply to the fractured bone, which would subsequently lead to atrophy and resorption of the segments [5]. Sometimes, this requires autogenous bone graft be used to reconstruct the buttress.
We have found that the K-wire technique is useful in the treatment of comminuted zygomatic fracture. It is also beneficial for patients with complex zygomatic fracture, for medically unstable or elderly patients. In the present study, we introduce a K-wire fixation technique for zygomatic fixation and assess its efficacy, safety, and clinical issues.
METHODS
Study patients
A retrospective review was performed for patients with zygomatic fractures at a single tertiary care institution between January 2010 and December 2013. Patients were included for comminuted fractures, elderly patients, medically unstable patients, and/or complex fractures. Patients who underwent open reduction and plate fixations were excluded from the review. Medical records were reviewed for demographic information, operative time, comorbidities, and postoperative outcomes including complications.
Surgical methods
Upon general induction and surgical preparation, the fractured bones were identified with palpation and outlined. Through a 2-cm horizontal incision, the frontozygomatic suture is identified around the bounds of the lateral eyebrow. After periosteal dissection, the zygomatic fracture was reduced using an elevator, hook, or Carroll-Girard type device. The fracture through or around this suture was fixed with a plate consisting of 5 or more fixation holes.
A 2-mm stab incision was made on the ipsilateral malar eminence. A 0.062-inch K-wire was inserted through deeper portion of the main fractured segment of zygomatic bone. If the plate fixation was insufficient in maintaining proper reduction, a Carroll-Girard screw was used through another stab incision prior to further advancement of the wire into the medial facial bones.
With the bones in reduced state, the wire was drilled further medially in a horizontal plane. The K-wire was advanced until it had crossed the maxillary bones and the nasal septum with the tip in the contralateral maxillary sinus. The location of the tip was estimated using an extra wire of the same length, placed over the face of the patient.
With zygomatic bone properly reduced and fixated, the exposed end of the K-wire was trimmed down to just above the skin. After 4 weeks, the wires were removed in outpatient setting without anesthesia.
Postoperative evaluation
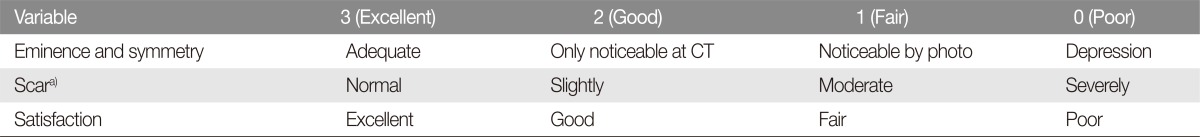
At the 6 months after each operation, three plastic surgeons (an attending and two resident physicians) evaluated the aesthetic outcomes for malar eminence/symmetry and K-wire site scar. These results were evaluated based on a 4-point scale (0 to 3 points). For malar eminence/symmetry, 3 points represented 'excellent result with satisfactory contour'. Two ('2') points represented 'adequate contour on photography but with a minimal undercorrection identified on radiographs'. A single (1) point was given for the 'presence of minimal asymmetry of malar contour'. A surgical outcome of 0 points represented a 'readily noticeable depression in the malar eminence'. As for the K-wire site scar, we evaluated the scar with only the pigmentation evaluation from the Vancouver Scar Scale (VSS) because rest of the VSS assessments were not applicable after the removal of the K-wire.
In addition to assessment by the surgical staff, the surgical outcome was evaluated by the patients themselves using a 4-point scale subjective satisfaction score. Individual patients were instructed to rate his/her satisfaction level from 0-to-3 points, where 3 points was 'excellent', 2 points as 'adequate', 1 point as 'fair', and 0 point as 'poor' (Table 1).
Medical records were also reviewed for the following postoperative complications: inflammation due to a K-wire, displacement of zygomatic bone, persistent cheek drooping, and maxillary sinus dysfunction. In addition, authors also examined the patients for the presence of diplopia, enophthalmos, infraorbital nerve paresthesia, lid malposition, need for plate removal, and/or trismus.
RESULTS
The review identified 25 patients meeting the inclusion criteria (21 males and 4 females; mean age, 52 years). The mean operation time was 43 minutes, and patients were followed for a mean of 6.2 months (range, 6 to 22 months). Eleven of the patients had complex fractures involving the frontal bone (3), naso-orbit-ethmoid bone (5), and mandibular bone (3).
Of the 25 patients, K-wire was sufficient by itself in maintaining reduction in 7 patients, with 18 patients requiring plate fixations in addition to K-wire fixation. Patients undergoing reduction with K-wire only had either severe underlying diseases or coexisting injuries (subdural hemorrhage, drug-resistant atrial fibrillation, colorectal cancer with systemic metastasis, hypotension during neurosurgery, and massive bleeding due to pelvic bone fracture. Also, an additional surgery could not be easily expected in the near future.
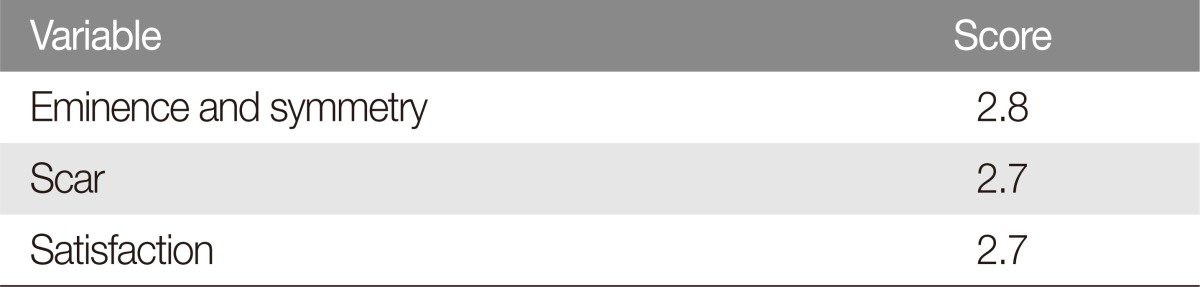
The mean score for malar contour was 2.8 points. The K-wire site scars received a mean score of 2.7 points. Patients reported an average of 2.7 points in satisfaction (between 'excellent' and 'good') (Table 2).
Overall, complications were infrequent and minimal. Transient paresthesia had occurred in two patients. This postoperative paresthesia resolved during the clinical follow-up period. There was one case of inflammation around the K-wire, which subsided with wire removal and without any further medical treatment required. No other complications were noted.
Case 1
A 70-year-old man slipped and fell at home and subsequently presented to the emergency room with comminuted right zygomatic fracture (Fig. 1). His pre-existing comorbidities included atrial fibrillation and osteoporosis. The patient underwent operative reduction 3 days after the injury.
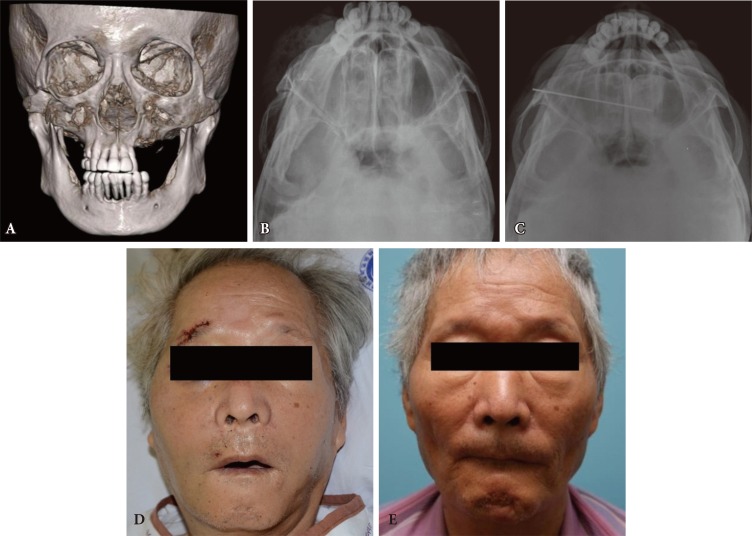
This 70-year-old man sustained a facial injury with comminuted right zygomatic fracture from falling. Preoperative facial 3-dimensional-computed tomography scan demonstrates osteoporotic changes in the zygomatic bone as well as partially edentulous maxilla and mandible (A). The preoperative zygomatic arch view shows a depression of the right zygomatic bone (B). The postoperative zygomatic arch view shows a single K-wire maintaining fixation of the zygomatic bone in the reduced position (C). The photographs are from before (D) and 6-month after the operation (E).
Upon general induction, the heart converted into an atrial fibrillation rhythm with relatively stable vital signs. To reduce the operative time, the zygoma was reduced using the Gillies method. The K-wire was inserted into the main fracture segment of the zygoma, which allowed increased manipulation of the fractured bones. With the zygoma reduced into a contour symmetric to the contralateral cheek, the K-wire was advanced until its tip was within the contralateral nasal cavity. Despite the atrial fibrillation, the patient tolerated the procedure and general anesthesia without any intraoperative complications and was eventually discharged home after an uneventful hospital course.
The K-wire was removed 4 weeks after the operation, and the skin healed well without any complications. At 6 month clinic visit, the operated cheek did not demonstrated any depression, and remained symmetric to the contralateral, non-injured cheek.
Case 2
A 20-year-old man was injured in a motorcycle collision and was transported to the emergency room (Fig. 2). The patient was found to have epidural hemorrhage and panfacial fractures, including comminuted right zygomatic fracture, bilateral mandibular fractures, nasal bone fracture, right orbital blowout fractures, frontal bone fracture. The epidural hemorrhage was managed by immediate decompressive craniotomy and removal of hematoma.

This 20-year-old man was injured in a motorcycle collision. In the trauma evaluation, he was found to have epidural hemorrhage and panfacial fractures, including comminuted right zygomatic fracture, bilateral mandibular fractures, nasal bone fracture, right orbital blowout fractures, frontal bone fracture. The epidural hemorrhage was managed by immediate decompressive craniotomy and removal of hematoma. The preoperative facial 3-dimensional-computed tomography scan shows a severe comminuted right zygomatic fracture (A). Two-point microplate and K-wire fixations were used to maintain the reduction of right zygomatic bone (B). The photographs are from before (C) and 8-month after the operation (D).
The patient did not suffer any complications and began to recover. Two days later, he was brought to the operating room for the facial bone fractures. The mandibular fracture was addressed first, with open reduction and internal fixation of left parasymphysis and the right angle fractures using miniplates. The zygomatico-maxillary buttress was severely comminuted, with too many small fragments to be fixed at the same time. Also, the operation ran for longer than expected, with the patient developing unstable vital sign. The zygoma was fixed in two points: at the zygomaticofrontal suture and at the inferior orbital rim. The blowout fracture was reconstructed with titanium plates. The midface bones were stabilized with a K-wire, which was removed 2 weeks later.
DISCUSSION
Various methods have been used in the management of zygomatic fractures, depending on the fracture pattern and severity [2]. Open approaches are generally followed by internal plate fixation, and this method is considered the standard treatment of zygomatic fracture [1]. One significant advantage of the open method is the potential use of three-point fixation at the zygomatico-frontal suture, the infraorbital rim, and the zygomaticomaxillary buttress [29]. This combination withstands the strong masticatory forces which are known to rotate the fractured segments downward, backward, and medially [1011]. The rigidity afforded by the stable fixation minimizes the risk of malunion and promotes early return to daily activities.
However, a three-point fixation has several disadvantages. Open reduction requires an incision scar and causes complications such as soft tissue injury and bone resorption due to the extensive dissection of periosteum [12]. In addition, the surgical technique is somewhat complex and time-consuming. The operation requires many operative equipment and is expensive. Small bone fragments could be lost during open reduction, and this often requires bone grafts. Rigid fixation by means of plating will be strictly fixed in place, so the reduction on the other sites will be affected by the previous rigid fixation [7].
In 1950, Fryer [4] reported the use of K-wire for zygomatic fracture. Since then, several authors have reported their own modification of the K-wire technique [6713]. The K-wire fixation method, although archaic, is used with consistency in certain types of zygomatic fractures. The operation is simple and fast. It lessens medical costs because of the minimal dependence on specialized equipment.
Disadvantages of the K-wire technique are unstable reductions, undercorrection, and inaccurate fixations. These are not direct consequences of the K-wire fixation itself but of the closed approach which does not allow visual confirmation of proper reduction. The addition of K-wire to internal plates have been shown to prevent non-union [5714]. Additional disadvantages is the potential for pain and infection around the exposed portion of the Kwire [23]. However, the discomfort associated with K-wire is transient, and these symptoms often fade away after removal of the wire. The K-wire should be inserted carefully, to avoid injury to the infraorbital nerve, orbital cavity, and dental root.
In this study, the operation time was short for K-wire fixation of the zygomatic; only a few minutes were required for inserting the K-wire. Patient satisfaction was high with a mean score of 2.8 points. No prolonged cheek drooping was observed in any of the patients. Cheek drooping occurs by soft tissue redundancy caused by extensive subperiosteal dissection and detachment from the insertion area of the masseter, zygomatic major and zygomatic minor muscles [15]. This drooping could be avoided by minimizing periosteal dissection and retaining as much of the attachments between bone and muscles.
Scarring was minimal at the site of K-wires. In one patient, the soft tissue around the exposed portion of K-wire showed signs of inflammation, but this resolved within two days of wire removal. Transient paresthesia was observed in two patients, which improved throughout the follow up period.
All patients treated with K-wire only were medically unstable and would tolerate a limited operating time. The K-wires preserved the periosteum of multiple bone segments, which reduce the displaced bones and provide stability to the malar-midface area. In these patients, forces of masticating muscles were assumed not to be strong because of severe co-morbid conditions. The operation result was usually acceptable if the prominent area was sufficiently reduced. The prominent area is the direct effect of perception on face and is more under aesthetical aspect more important than the other area. Some misalignment in the other area could be frequently negligible because the facial bone is covered by thick skin and soft tissues [15].
In more medically stable patients, the K-wire was used in addition to plate fixation. The K-wire alone cannot adequately fixate the zygoma in severe or unstable displacement of the zygomaticofrontal suture or infraorbital rim. The K-wire technique is an alternative method to plate fixation of the zygomatico-maxillary buttress. Using this technique, we were able to preserve the periosteum in the zygomatico-maxillary area and save the operating time. As periosteum dissection decreases blood supply, the percutaneous K-wire fixation was found to be more advantageous in terms of maintaining the blood supply to the bone. For this reason, the use of K-wires as an adjunct to additional fixation methods (i.e., plates) appears advantageous.
The K-wire might appear to be an antiquated method, and it does have disadvantages associated with inadequate mechanical fixation. However, we have found that the K-wire offers a good approach to treating comminuted zygomatic fractures. Specially, this method is very beneficial for medically unstable patients who cannot tolerate prolonged operation time. Also, the technique is appropriate in elderly patients in whom screws and plates may loosen in osteoporotic bony cortex.
Notes
No potential conflict of interest relevant to this article was reported.