Direct Open Venous Drainage: An Alternative Choice for Flap Congestion Salvage
Article information
Abstract
In this report, we present a scalp defect reconstruction with lateral arm free flap. We highlight the difficulty in obtaining a recipient vein and the venous drainage managed through an open end of the donor vein. A 52-year-old woman presented with a pressure sore on the left scalp. A lateral arm free flap was transferred to cover this 8×6 cm defect. The arterial anastomosis was successful, but no recipient vein could be identified within the wound bed. Instead, we used a donor venous end for the direct open venous drainage. In order to keep this exposed venous end patent, we applied heparin-soaked gauze dressing to the wound. Also, the vein end was mechanically dilated and irrigated with heparin solution at two hour intervals. Along with fluid management and blood transfusion, this management was continued for the five days after the operation. The flap survived well without any complication. Through this case, we were able to demonstrate that venous congestion can be avoided by drainage of the venous blood through an open vessel without the use of leeches.
INTRODUCTION
The scalp is a structure which covers the skull, ranging from the hair line on the forehead, to the occipital region. The scalp consists of skin, subcutis fat, the galea-aponeurotica, loose connective tissue, and the periosteum. Scalp may be damaged for congenital factors or through various acquired conditions and injuries such as cancer, trauma, pressure sores, infections, and burns. The galeaaponeurotica and the periosteum is very fibrous and resists stretching. Because of this, scalp defects can be closed primarily only if the defect measures less than 3 cm in diameter.
According to Beasley et al., defects larger than 3 cm can be repaired using tissue expanders, local flap, regional flap, skin graft, or free flap, depending on the position and size of defect, aesthetic requirements, exposed structures, underlying disease, and operational history [1].
In the past, the free flap method was not used frequently, due to the long operation time, the complexity of the procedure, and potential defects caused by micro-vascular complications. However, advances in micro operation and postoperative care have overcome several of these weaknesses, and free flap transfers has become popular in scalp reconstruction [2].
Among the various free flaps available for scalp reconstruction, lateral arm free flap is ideal. It offers adequate padding with a sliding fascia. The texture and color of the skin matches the scalp well, and donor-site morbidity is relatively low. For these reasons, we frequently choose the lateral arm free flap to reconstruct scalp defects. In this report, we present a scalp defect reconstruction with lateral arm free flap. We highlight the difficulty in obtaining a recipient vein and the venous drainage managed through an open end of the donor vein.
CASE REPORT
A 52-year-old female presented to the plastic surgery clinic with a chronic open wound in the left temporal lesion. Five months prior to this, the patient had undergone craniectomy for an acute subdural bleeding. The patient gradually recovered and underwent reconstructive cranioplasty two months prior to the presentation to the clinic.
On exam, a pressure sore measuring 6×4 cm was located in the left temporal region (Fig. 1). There were severe scarring near the lesion caused by previous operations. The location and size of the defect precluded many local flap options, and the patient consented to a free flap reconstruction of the soft tissue defect. The patency of superficial temporal artery was confirmed using a hand-held Doppler, and the superficial temporal vein was assumed to follow the course of this artery.
Under general anesthesia, the wound was debrided, after which the defect measured 8×6 cm. The wound was carefully explored, and the superficial temporal artery was followed from a proximal to distal course until we were able to find an appropriate recipient vessel about 3 cm away from the inferolateral margin of the defect.
A 8.5×6.5 cm fasciocutaneous flap was elevated in a spindle shape from the left lateral arm. The flap included a 1-mm diameter artery and two veins. The donor site was closed primarily, and the harvested flap was attached to the defect using a 4-0 nylon stay suture. Under a microscope, the flap artery was anastomosed to the frontal branch of the superficial temporal artery, but no recipient vein could be identified. Because of this, we decided to use one of the veins as a drainage channel. This adventitia of the venous end was fixed to the skin using 9-0 nylon. The remaining border of the wound was closed with temporary drains in place.
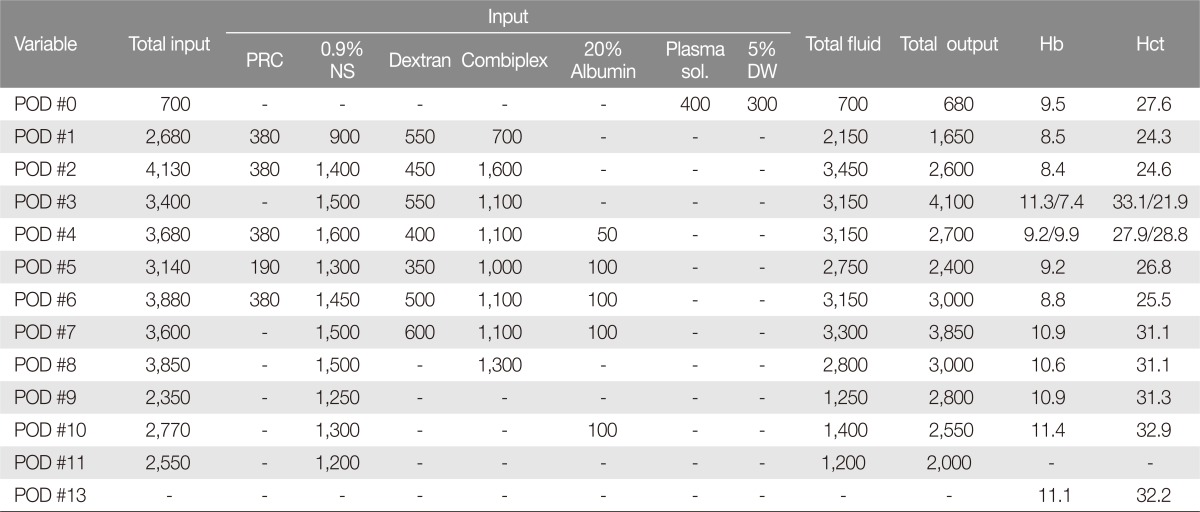
Postoperatively, the patient was initially managed in the intensive care unit. Postoperative hemoglobin and hematocrit were 9.5 and 27.6, respectively, and these values were kept within 8-10 and 25-30 range with daily blood counts and transfusions as needed. The exposed venous end was kept moist under heparin soaked-gauze dressing. Every 2 hours, the vein end was also mechanically dilated and irrigated using 400 IU/mL heparin-Na solution. The heparin gauze was replaced. This was continued for five days (Fig. 2).

Intraoperative illustration. The arterial anastomosis was successful, but no recipient vein could be identified. An open end of a flap donor vein was drained directly outside the skin suture.
In order to estimate the blood loss during the operation, we measured the weight of blood-soaked gauze. The amount within the gauze was 40-90 g (Fig. 3).

Immediately after the reconstruction. The open end of the vein was monitored every 2 hours for continued blood drainage (red arrow).
Postoperative care included aggressive fluid therapy (Dextran®), an infusion of heparin and Eglandin®, and a blood transfusion (9 units of packed red blood cells for 5 days after operation). The hemoglobin was maintained within the targeted hemoglobin range (range, 8.4-9.5; except 7.4 on postoperative day 3) (Table 1). After five days, the vein was no longer dilated and irrigated. The flap continued to be perfused without any signs of congestion. We considered clamping the vein end, but this was considered unnecessary as the vein appeared to have closed spontaneously. The subcutaneous drains were removed on postoperative day 9. The flap survived well without any complications (Fig. 4).
DISCUSSION
Venous congestion is more common than arterial insufficiency after free flap transfer. Improperly managed venous congestion may result in flap necrosis. In order to prevent flap necrosis due to congestion, the flap should be allowed to drain the venous blood for 2-10 days after an operation in which venous revascularization occurs. In the case presented, we decided to use an open end of a vein to provide the blood flow out of the flap, by which the blood drained to outside of the skin. The vein required intermittent mechanical dilatation and heparin irrigation [3].
At the same time, we monitored the patient for vital signs and clinical symptoms of hypovolemia. When the effective blood volume had decreased, the patient was given replacement packed red blood cells and fluid. Similar to other reconstruction surgeries, such nasal tip, fingers and penis, small sized flaps could survive without venous anastomosis [345]. In these situations, the classic method employed heparin-soaked gauze dressing on exposed suture line or de-epithelialized area to decrease venous congestion in the flap.
The lateral arm free flap is usually a good reconstructive choice for large scalp defects. However, the recipient vessel in the temporal area could not be found, which was most likely a consequence of previous operations. Because of this, we used the donor venous end for drainage, to enable congestion salvage. In spite of the venous congestion risk, the flap was successfully taken without the use of leeches. This method is a less expensive and safer alternative to using leeches. In addition, it does not leave a noticeable scar on the flap.
The present case suggests that a lack of venous coupling can be managed with direct open venous drainage and intensive postoperative care.
Notes
No potential conflict of interest relevant to this article was reported.