Mucosa-associated lymphoid tissue lymphoma on right lower eyelid previously diagnosed as lymphoid hyperplasia
Article information
Abstract
Mucosa-associated lymphoid tissue (MALT) lymphoma is an uncommon form of non-Hodgkin lymphoma involving the mucosa-associated lymphoid tissue. Most commonly affected organ is the stomach. But, it could affect almost every organ in the whole body. If they have suspicious lesion, excision biopsy could be made. For staging, blood test including blood smear, abdomen and chest tomography or scan will be checked. Also, bone marrow test can be done if it is needed. The patient had visited the clinic for palpable mass on right lower eyelid. With excisional biopsy, it was diagnosed as lymphoid hyperplasia on pathologic test. But 2 years later, the patient came with recurrent symptom for our department with worry. At that time, we recommended excisional soft tissue biopsy under general anesthesia. Unfortunately, it was revealed MALT lymphoma on pathologic finding. It turned out to be stage 3 in Ann Arbor staging system without B symptoms. Hematologic consultation was made and she was treated with adjuvant chemotherapy for eight cycles to complete remission. We report a case of MALT lymphoma on subcutaneous tissue at right lower eyelid previously diagnosed as lymphoid hyperplasia.
INTRODUCTION
Mucosa-associated lymphoid tissue (MALT) lymphoma is an uncommon form of non-Hodgkin lymphoma (NHL) involving the mucosa-associated lymphoid tissue. In the World Health Organization classification, it is listed as a malignant lymphoma. Most commonly affected organ is the stomach. But, it could affect almost every organ in the whole body. If they have suspicious lesion, excision biopsy could be made. For staging, blood test including blood smear, abdomen and chest tomography or scan will be checked. Also, bone marrow test can be done if it is needed. The patient visited the clinic for palpable mass on right lower eyelid. And it was revealed as lymphoid hyperplasia on pathologic findings. But 2 years later, the patient came with recurrent symptom for our department with worry. We recommended excisional soft tissue biopsy. Unfortunately, it was revealed as MALT lymphoma on pathologic finding. We report a case of MALT lymphoma on subcutaneous tissue at right lower eyelid previously diagnosed as lymphoid hyperplasia.
CASE REPORT
A 56-year-old female was presented with recurred palpable mass with 1×1-cm-sized on her right lower eyelid. She had visited a clinic for palpable mass on right lower eyelid 2 years before. With excisional biopsy, it was diagnosed as lymphoid hyperplasia on pathologic test (Fig. 1A). But with enhanced neck computed tomography (CT), the radiologist recommended a further evaluation because it couldn’t rule out malignant lymphoma for ambiguous haziness around a mass. As she had refused an additional examination for ruling out malignant lymphoma, any further exam was not proceeded and follow-up check was loss for 2 years.
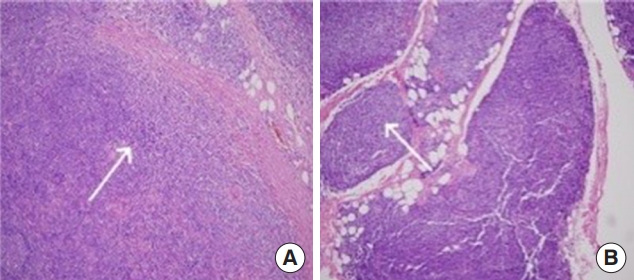
(A) In the first biopsy of 2 years ago, it was revealed as lymphoid hyperplasia with proliferation of lymphocyte but there is no bizarre patterns (arrow; H&E, ×100). (B) In the final biopsy, bizarre nodular infiltration and differentiations of lymphocyte was observed with forming lymphoepithelial lesion (arrow; H&E stain, ×100). After all, it turned out to be mucosa-associated lymphoid tissue lymphoma.
In this visit, she complained the recurrent palpable mass with growing and also wanted to excisional biopsy to know exactly what it is. The patient underwent excisional biopsy at the same site of right lower eyelid again with general anesthesia. In the operation, a yellowish oval-shaped mass was found adhered to orbicularis oculi muscle which was confused with fat mass from right lower eyelid was revealed as MALT lymphoma on pathologic finding (Fig. 1B). Immunohistological stain showed that CD20, CD79a and reactive CD3-positive T cells were positive. But cyclin D1 was negative. Complete blood count showed normal leukocyte count and neutrophil count. Liver function tests, lactate dehydrogenase (LDH), beta-2-microglobulin, and serum protein electrophoresis were normal. Serologic tests for human immunodeficiency virus, hepatitis B virus, and hepatitis C virus (HCV) were negative. Serology studies for Chlamydia psittaci, Chlamydia trachomatis, and Chlamydia pneumoniae were negative. Immunoglobulin E (IgE) level was normal. There was no clinical or laboratory evidence of pre-existing autoimmune disease.
Consulting with hematologist, the positron emission tomography-computed tomography (PET-CT) and enhanced neck CT was performed after operation to tumor staging and showed stage III MALT lymphoma with invasion of both cervical and abdominal lymph node in Ann Arbor staging system (Fig. 2). Also the patient have no B symptoms. At a bone marrow biopsy, karyotype was normal, without bone marrow involvement. The patient received eight cycles of rituximab, cyclophosphamide, vincristine, and prednisone with complete remission for 2 years.
DISCUSSION
MALT lymphoma usually originates from B lymphocyte that occurs in reactive lymphoid tissue with secondary inflammation. Most commonly affected organ is the stomach. But, this type of disease may affect orbit, ocular adnexa, intestine, lung, salivary gland, thyroid, and skin [1]. In fact, 5% of all NHL patients was affected on ocular adnexa. Interestingly, 15%–20% of these are aggressive (diffuse large B cell mantle cell lymphoma) and 80%–85% of these are indolent (follicular or MALT type) [2].
The ocular adnexal extranodal marginal zone lymphoma is rare and usually presents with localized disease rather than systemic disease [3]. Bilateral involvement was reported in 10%–15% of the cases [4]. Histologically, it is characterized by proliferation of colonization of reactive germinal centers, lymphoepithelial lesion, bizarre epithelial infiltration and differentiation of plasma cells. The MALT lymphoma concept suggests that this type of tumors are usually arise from chronic stimulated lymphoid tissue by prolonged infections and/or autoimmune diseases and correspond to cells of postfollicular differentiation stages [5,6].
Chronic inflammation plays a huge role with exogenous and endogenous antigens. Usually this type of tumors have association of Helicobacter pylori with gastric diseases, Borrelia burgdorferi with cutaneous tumors, C. psittaci with ocular adnexal MALT lymphoma [7,8]. A case of extranodal marginal zone lymphoma of the ocular adnexae and subcutaneous involvement in association with chronic HCV infection was reported [9].
In fact, patients with this type of tumors have high prevalence of Sjogren syndrome, Hashimoto thyroiditis such as thyroid gland and salivary gland, respectively and also other autoimmune diseases. This can be the hypothesis that endogenous antigens could be the trigger to the tumor formation for that site by means of inflammatory reactions resulting abnormal activation of NF-kB pathway and uncontrolled B-cell expansion [10]. In these days, some studies revealed that Immunoglobulin G4 (IgG4) sclerosing disease is associated with lymphoproliferative disorders. Middle aged men is more affected by multiple benign mass. The pathogenesis is unknown, it is believed to be autoimmune. But, primary cutaneous marginal zone lymphomas have high IgG4 expression (39%), noncutaneous MALT lymphomas, located in ocular adnexa, rarely expressed IgG4 [11].
Genetical aberration is associated with MALT lymphomas. It is also seen some structural chromosome abnormalities and numeric abnormalities. Almost trisomies and translocations. For examples, the t(1;14)(p22;q32), t(11;18)(q21;q21), t(14;18) (q32;q21) and trisomies 3 and 18. It is largely related to MALT lymphoma.
Ocular adnexa, orbit, skin and salivary glands mainly express the t(14;18)(q32;q21), but pulmonary and gastric tumors mainly express the t(11;18)(q21;q21). The t(14;18)(q32;q21) is most frequently observed chromosomic translocation and it is strongly related to MALT lymphoma, also expressed in rare cases of extranodal diffuse large B-cell lymphoma. Chromosome 3 trisomy is usually involved with aged >50 years and the orbital involvement is diagnosed about 81% out of all cases. But chromosome 18 trisomy is usually involved with aged <50 years and the conjunctival involvement is frequently diagnosed [12,13].
Management of MALT lymphoma depends on the organ involvement and the stage of disease. For NHL’s staging, the 1971 modified Ann Abor staging system is usually considered.
Four disease stages are: an involvement of a single lymph node region (stage I) or a single extra-lymphatic site (stage I E), an involvement of two or more lymph node regions on the same side of the diaphragm (stage II), involvement of lymph nodes in both sides of the diaphragm±extra-lymphatic site±spleen or both (stage III, sage III E, stage III S, stage III ES), a disseminated disease (stage IV).
Also, two subgroups can be distinguished based on symptoms: (A) for asymptomatic patients, and (B) for patients with unexplained weight loss of more than 10% of body weight in the months previous to admission, unexplained fever with temperature above 38°C and night sweats [14]. But there is some limitation of disease staging for modified Ann Arbor staging system like prognostic difference of affected regional variations. Therefore, a new TNM-based staging system was oriented for primary orbital adnexa lymphomas under the auspices of the American Joint Committee on Cancer [15].
Treatment of MALT lymphoma requires a multidisciplinary approach including surgeon, radiotherapist and hematologist. In most patients, local treatment including radiation therapy or surgery may be adequate to deal with the disease. But, if the disease has spread or has been refractory on antibiotics, chemotherapy may need to be considered. Excisional biopsy of mass is essential procedure not a complete curative purpose but a diagnosis of MALT lymphoma because it could help for immunophenotyping analysis or histological confirm. When simple excision alone as complete curative treatment of MALT lymphoma is dangerous because it could tend to local relapse more frequently than radiotherapy alone. So, the role of surgery is limited a side of diagnostic tools not a total curative [16]. Radiotherapy for lymphoma is considered the standard treatment of local involvement of this disease without disseminations. Also, it is proven that radiotherapy could control the local relapse of the disease regardless of its types of lymphoma. In latest study, 77 patient treated with radiotherapy alone over a period of 20 years showed a 5 years and 10 years overall survival of 97.6% and 93.5% respectively [17]. But obviously, complications of radiotherapy for ocular area are shown up for ocular toxicity in forms of immediate and late complications. Immediate complications are presented by conjunctivitis or eyelid irritations. Late complications are included for retinal vasculopathy, optic neuropathy, cataract formations [18]. Chemotherapy for treatment of MALT lymphoma could be used that single agent (chlorambucil, fludarabine, and pentostatin) or CVP regimen (cyclophosphamide, vincristine, and prednisone) intended for low toxicity. It is utilized systemic involvement or not. Sasai et al. [19] suggested no meaningful difference in overall survival rate for patient with MALT lymphoma comparing effectiveness of radiotherapy with single agent chemotherapy and combination chemotherapy. It seems that adjunctive chemotherapy treatment with radiotherapy did not add any benefits than chemotherapy treatment alone. An overall 5-year survival rate of this disease is ranging between 54% and 94% depending on studies. There is some positive and negative prognostic factors. The positive prognostic factors are limited disease, good performance status and absence of systemic symptoms. Also, It is revealed that risk difference of primary site of presentation including conjunctival tumor shown lowest risk but eyelid tumor shown highest risk. The negative prognostic factors are advanced staged disease, 60–64 years aged, nodal involvement, elevated serum LDH level [16,19,20]. Because of ambiguous CT findings, we recommended further evaluation despite of a first biopsy finding revealed with lymphoid hyperplasia. A patient denied another studies at all. By doing so, it was delayed proper diagnosis and treatment of this malignancy. Therefore, the authors recommend further evaluation or closed follow-up to a patient with any doubtful pieces whether pathologic findings were benign like lymphoid hyperplasia or not as we reported.
Notes
No potential conflict of interest relevant to this article was reported.
Ethical approval
The study was performed in accordance with the principles of the Declaration of Helsinki. Written informed consent was obtained.
Patient consent
The patient provided written informed consent for the publication and the use of her images.

