Orocutaneous fistulas of odontogenic origin presenting as a recurrent pyogenic granuloma
Article information
Abstract
Orocutaneous fistulas, or cutaneous sinuses of odontogenic origin, are uncommon but often misdiagnosed as skin lesions unrelated to dental origin by physicians. Accurate diagnosis and use of correct investigative modalities are important because orocutaneous fistulas are easily confused for skin or bone tumors, osteomyelitis, infected cysts, salivary gland fistulas, and other pathologies. The aim of this study is to present our experience with a patient with orocutaneous fistulas of odontogenic origin presenting as recurrent pyogenic granuloma of the cheek, and to discuss their successful treatment.
INTRODUCTION
Orocutaneous fistulas, or cutaneous sinuses of odontogenic origin, are a rare condition and diagnosis is challenging. They are often misdiagnosed by physicians as skin lesions or nonodontogenic lesion because they are easily confused for skin or bone tumors, osteomyelitis, infected cysts, salivary gland fistulas, and other pathologies [1]. We present a patient with orocutaneous fistulas presenting as a recurrent pyogenic granuloma (PG) of the cheek, which was initially misdiagnosed as a nonodontogenic lesion. We emphasize that accurate diagnosis and use of correct investigative modalities are important for prompt treatment and for reducing recurrence and complication rates.
CASE REPORT
A 74-year-old female patient visited Inje University Haeundae Paik Hospital with a chief complaint of a pinkish mass on her right cheek of 3 months’ duration. A history of the presenting illness revealed that the growth was gradual in onset, and mass was initially small but grew to the present size. The growth measured approximately 0.3 cm×0.3 cm in diameter and was soft to firm in consistency (Fig. 1). The skin lesion was painless and asymptomatic, except for the slight discomfort of the patient due to the growth. There was no evidence of pus discharge from the lesion. Intraoral examination showed no other mass lesions, fistula, or gingivitis. No relevant medical history was obtained from the patient and her family.
The skin lesion was completely excised under local anesthesia and sent for histopathological examination. The subsequent skin defect was covered by bilateral V-Y advancement flaps. Fig. 2 shows the immediate postoperative appearance, which confirms that the skin defect was covered without any tension. Histopathologically, hematoxylin and eosin staining confirmed the diagnosis of PG (Fig. 3). The healing period was uneventful, but 2 months after surgery, the patient returned to our clinic with persistent discharge from the previous wound site. A second surgery was performed to excise the recurrent skin lesion. A unilateral V-Y advancement flap was used for the coverage of the skin defect (Fig. 4). Similar to the initial surgery, there was no problem with wound healing. However, 1 month later, she returned to our clinic with a complaint of persistent discharge. A wound culture test was performed but no bacteria were identified. For histopathological examination, a tissue biopsy was performed and the results revealed chronic inflammation and abscess formation.

Immediate postoperative photo showing complete elimination of the mass by the bilateral V-Y advancement flap.
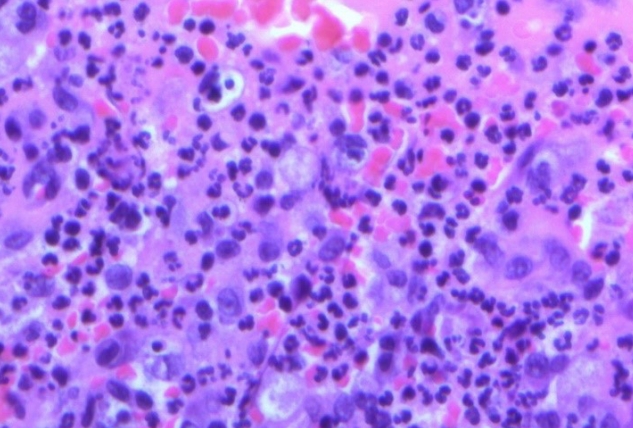
Histopathologic examination of the lesion shows that it consists of condensed small-caliber vessels with scattered red blood cells. The stroma is fibromyxoid with scattered inflammatory cells. Cytologic atypia and mitoses are observed (H&E, ×400).
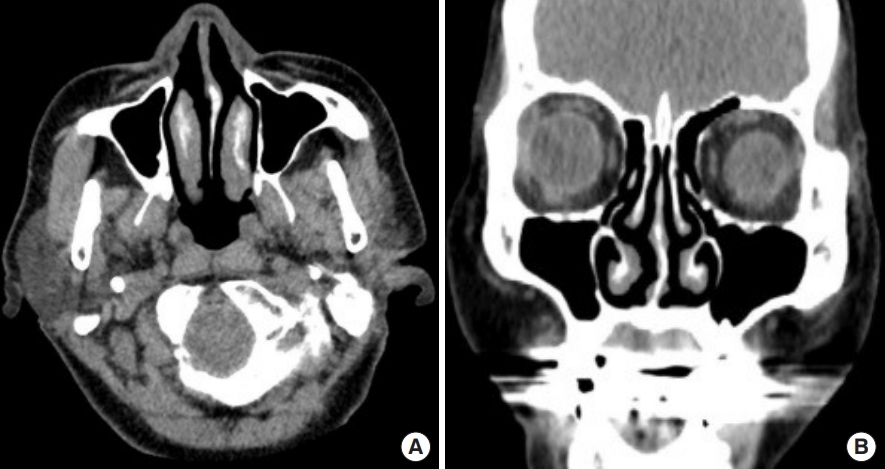
In order to identify the cause of the recurrent PG, intraoral examination was repeated. There were no findings suggestive of odontogenic infection. Subsequently, panoramic X-ray and computed tomography (CT) were performed. The panoramic radiograph revealed partial alveolar bone loss due to pulpitis and the presence of a periapical abscess of the right maxillary canine tooth (Fig. 5). However, there were no findings suggestive of chronic osteomyelitis, such as soft tissue swelling, mucosal abscess, cutaneous abscess, and draining fistulas, on the CT images (Fig. 6). For evaluation of the odontogenic infection, the patient was referred to the dental department. During dental evaluation, irreversible pulpitis was observed on the right maxillary canine tooth. Therefore, the tooth was extracted and systemic antimicrobial therapy was started to suppress the odontogenic infection. The patient visited our clinic 2 weeks after the extraction, and no secretions from the cheek flap site were found and wound healing was complete. After 3 months, all odontogenic infections had resolved and no further recurrence was observed (Fig. 7). The extracted tooth was replaced with a dental implant.

Panoramic view of dental computed tomography images showing partial alveolar bone loss and periapical abscess formation in the right maxillary canine teeth.
DISCUSSION
PG, also known as lobular capillary hemangioma, is a benign proliferative vascular tumor of the skin or mucous membranes that is characterized by rapid growth and a friable surface [2]. In fact, the term “pyogenic granuloma” is a misnomer as it does not contain pus and is not, strictly speaking, a granuloma histopathologically [3]. Although the cause of PG is unknown, it is thought to be a hyperplastic and neovascular response to angiogenic stimuli, such as chronic low-grade local irritation, traumatic injury, hormonal factors, or certain drugs [4].
Clinically, PG is a smooth or lobulated exophytic lesion manifesting as a small, red, erythematous papule on a pedunculated or sometimes sessile base, which is usually hemorrhagic and compressible [5-7]. The size varies in diameter from a few millimeters to several centimeters, but is usually less than 2.5 cm [8]. It can grow rapidly and will often bleed profusely with little or no trauma. It may be found in the oral cavity or extraorally. Intraorally, the gingiva is the most common site of involvement (approximately 60%–70%), followed by the lips (14%), tongue (9%), buccal mucosa (7%), and palate (2%) [9]. Histopathologic confirmation is helpful for making a definitive diagnosis. There are several different treatment modalities, such as surgical excision, which is the treatment of choice, and laser therapy, electrocautery, cryotherapy, sclerotherapy, steroid injection, and intralesional therapies using chemicals [4]. Recurrence is observed in up to 16% of patients after surgical excision of the PG lesions and secondary operations are mandatory [5-7]. This is believed to result from incomplete excision, failure to eliminate etiologic factors, or reinjury to the area. Therefore, the stimulating factors, if present, should be prevented, eliminated, or discontinued prior to the treatment to ensure successful outcomes.
Our patient had a recurrent PG of the cheek that recurred even after secondary excision. The patient had dental complications that caused loss of the alveolar bone and periapical abscess formation. The development of PG may have resulted from the persistent local trauma in the gap between the alveolar bone and canine tooth. In addition, the lack of adequate keratinized mucosa may have allowed the entrapment of soft tissue inside the gap, and contributed to the development of the PG. PGs associated with dental complications are thought to be capable of disseminating to the cheek region, causing external skin lesions. After the canine tooth was extracted and the odontogenic infection was completely resolved, the cheek flap healed spontaneously without recurrence.
Orocutaneous fistulas of odontogenic origin are often misdiagnosed by physicians and confused for skin or bone tumors, osteomyelitis, infected cysts, salivary gland fistulas, and other pathologies [1]. Our successful treatment strategy emphasizes the importance of the diagnosis with careful history-taking, meticulous examination, and radiographic examination with the awareness of odontogenic origin. In conclusion, treatment of orocutaneous fistulas of odontogenic origin should be combined with the elimination of any present provoking factors to ensure a successful outcome and prevent recurrence.
Notes
No potential conflict of interest relevant to this article was reported.
Ethical approval
The study was performed in accordance with the principles of the Declaration of Helsinki. Written informed consent was obtained.
Patient consent
The patient provided written informed consent for the publication and the use of her images.