Oblique transnasal wiring canthopexy via Y-V epicanthoplasty for telecanthus correction in a patient with Waardenburg syndrome
Article information
Abstract
Telecanthus is a common symptom accompanied by Waardenburg syndrome, a rare genetic disorder. The optimal surgery for telecanthus correction is still debated. A 28-year-old patient with Waardenburg syndrome underwent transnasal wiring canthopexy using a Y-V epicanthoplasty for telecanthus correction. A Mini-Monoka stent was used to prevent damage to the lacrimal apparatus. The intercanthal distance decreased from 50 mm to 43.2 mm. The easily designed Y-V epicanthoplasty incision provides sufficient operative field for oblique transnasal wiring, which is effective in properly positioning the medial canthal tendon. It has minimal scarring resulting in satisfactory cosmetic outcomes.
INTRODUCTION
Waardenburg syndrome (WS) is a rare genetic disorder that is often described as an autosomal dominant inherited disorder of the neural crest cells. It occurs in one out of 42,000 persons and is characterized by the following six symptoms: lateral displacement of the medial canthus (telecanthus), prominent broad root of the nose, hypertrichosis, heterochromia, deafmutism, and white forelock [1]. Although mutations in the PAX3, EDN3, EDNRB, MITF, SNAI2, and SOX10 genes are thought to be related to WS, diagnosis is made according to symptoms and family history [2]. There is no actual cure for WS and the treatment is mainly symptomatic.
Telecanthus, the most common symptom accompanied by WS, requires cosmetic correction [3]. Other causes of telecanthus may be trauma, tumor resection, congenital malposition, or aging. Numerous surgical procedures have been attempted to treat telecanthus, including transnasal wiring, screw fixation, interfragment wiring, and medial canthoplasty [4,5]. However, no consensus has been reached on the optimal surgical intervention. The methods used previously for the correction of telecanthus were often challenging because of incomplete correction, recurrence, and injury to the lacrimal apparatus, as well as other disadvantages such as conspicuous scar formation, a higher risk of bleeding, and prolonged operative time [6].
The method how to treat telecanthus in this case was introduced on author’s previous journal (Kim et al. [7]). In previous journals, most of cases were about treating in patients with trauma, but the authors found that this method is also useful for treating telecanthus accompanied by congenital disease. Patient’s consent was obtained for use of her clinical and radiological photographs for academic and research purposes. This study was approved by the Institutional Review Board (IRB) of Yeungnam University Hospital and adhered to the Declaration of Helsinki.
CASE REPORT
A 28-year-old woman who had been diagnosed with WS at another hospital was referred to us for correction of telecanthus. The patient also had a prominent broad root of the nose and had undergone augmentation rhinoplasty in another hospital. She did not have a pigmentation abnormality (heterochromia) of the iris, whereas it was observed in her sister who accompanied her. The patient’s interpupillary distance was 80 mm and the intercanthal distance was 50 mm.
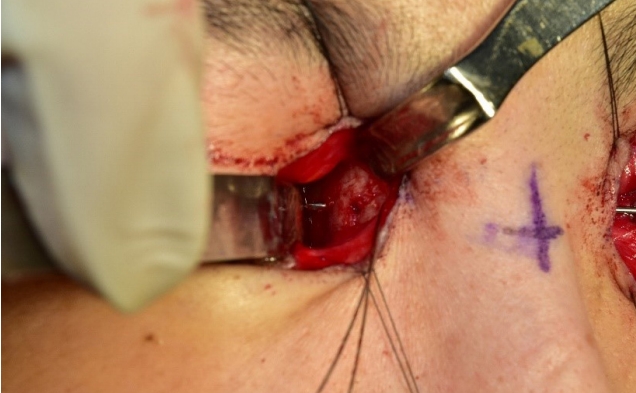
Surgery was performed under general anesthesia. Preoperatively, a Mini-Monoka (FCI, Cedex, France) monocanalicular stent was inserted into the lacrimal duct to prevent damage to the lacrimal apparatus. A Y-shaped epicanthoplasty incision (Fig. 1) was made and dissection was carried out into the medial orbital wall. On each side, two holes were made by drilling with a K-wire in the opposite nasal recession (Fig. 2). A 2-0 wire suspended medial canthal tendon (MCT) and was passed through the two holes. Thereafter, the wire was pulled and twisted until the MCT was firmly fixed on the superior and posterior regions of the opposite lacrimal fossa. The end of twisted wire was bent to avoid irritation to soft tissue. The medial canthal skin was sutured in a V-shaped manner. Mini-Monoka stent was removed after surgery.
After 9 months of follow-up, the intercanthal distance decreased from 50 mm to 43.2 mm (6.8 mm) (Fig. 3). There were no surgical complications such as recurrence, eye damage, scarring, or infection. Epiphora occurred transiently after the operation; the symptoms improved following the reinsertion of Mini-Monoka stent to lacrimal duct and keeping it in place for 3 months. The patient was satisfied with the aesthetic outcomes.
DISCUSSION
WS is a newly described syndrome that involves developmental anomalies of the eyelids, eyebrows and nose root, pigmentary defects of the iris and hair of the head, and congenital deafness. The most common symptom among these is telecanthus.
Numerous surgical procedures have been attempted to treat telecanthus, without a consensus on the optimal technique. The reason may be because telecanthus correction has been a challenge as it is often difficult to fix the MCT to the proper point of the orbit, resulting in incomplete correction and recurrence due to loosening of the tendon. Among the available techniques, oblique transnasal wiring is easily performed and has few complications [6]. Traditionally, coronal incisions and open sky techniques have been used for fixation of the MCT, because these methods can provide a good operative field. However, these methods often leave conspicuous scars and web contractures in the medial orbital regions, making it difficult to obtain satisfactory cosmetic results. We used an epicanthoplasty incision to overcome this problem. Compared to the two aforementioned methods, an epicanthoplasty incision does not provide a wider operative field. However, this method can provide a sufficient operative field to perform the transnasal wiring and it can increase the cosmetic satisfaction by leaving a minimal scar. In addition, the dissection and closure are not extensive, and the duration of operation can be shortened.
In this patient, epiphora developed even though we did not injure the lacrimal apparatus during surgery. Epiphora in this patient was temporary and improved after retaining the Mini-Monoka stent for 3 months. The reason may be because epiphora can be caused by crushing injury of the soft tissue around the lacrimal duct without direct injury to the lacrimal apparatus [8]. Temporary lacrimal sac compression by postoperative edema or repositioning of the MCT may also contributed to epiphora [9]. Temporary stenting or dacryocystorhinostomy can be used to treat epiphora. Among the temporary stents, Mini-Monoka stent is widely used because it is easy to use without foreign body sensation or discomfort [10]. Although temporary epiphora is considered a minor problem, the surgeons have to sufficiently explain about possibility of epiphora before surgery.
In conclusion, the Y-V epicanthoplasty incision is easy to design, and has minimal scarring as well as decreased operation time. The oblique transnasal wiring technique is effective for properly positioning the MCT and avoiding injury to the contralateral medial orbit. When performing this surgery, one should be aware of potentially damaging the inferior lacrimal apparatus. It can be prevented by inserting a Mini-Monoka stent.
Notes
Conflict of interest
No potential conflict of interest relevant to this article was reported.
Ethical approval
The study was approved by the Institutional Review Board of Yeungnam University Hospital (IRB No. 2019-10-045) and performed in accordance with the principles of the Declaration of Helsinki. Written informed consent was obtained.
Patient consent
The patient provided written informed consent for the publication and the use of her images.
Acknowledgements
This study was supported by the 2016 Yeungnam University Research Grants.