Is the retroauricular region a suitable donor site for full-thickness skin grafting in the era of mask wearing?
Article information
Abstract
Background
During the coronavirus disease 2019 (COVID-19) pandemic, the everyday use of face masks massively increased to prevent the spread of infection. Many people complain of ear pain and erosion when wearing a mask for extended periods of time. If prolonged mask usage is uncomfortable for ordinary people, a question arises—how much more inconvenient must mask wearing be for patients with a full-thickness skin graft (FTSG) donor site in the retroauricular region? Herein, we evaluated complications related to face mask use in 27 patients with a retroauricular FTSG donor site, with the goal of clarifying whether the retroauricular region is still an appropriate FTSG donor site in the context of the COVID-19 pandemic.
Methods
Complications in 27 patients treated by FTSGs harvested from the retroauricular region from 2019 to 2021 were investigated. A questionnaire comparing the normal and the operated sides was administered. Pain, itching, soreness, deformity, and symmetry were further investigated.
Results
Pain and itching were the only observed complications. The operated side was slightly more painful than the normal side in four patients (14.8%), and four patients (14.8%) reported itching on the operated side. However, all patients who experienced complications stated that the pain or itching did not interfere with mask wearing. Most symptomatic patients were older than 60 years of age (23.8%, p=0.185) and wore masks for longer periods of time (28.5%, p=0.326).
Conclusion
Few retroauricular donor site-related complications occurred, and none of these complications caused inconvenience in daily life. Therefore, in the COVID-19 pandemic, the use of the retroauricular region as an FTSG donor site remains appropriate.
INTRODUCTION
Coronavirus disease 2019 (COVID-19) was declared a global pandemic in 2020 after being first reported at the end of 2019. The World Health Organization declared the outbreak to be a public health emergency in January 2020. The virus is transmitted through two main routes: direct and indirect [1,2]. The high infectivity and pathogenicity of COVID-19 have led to radical changes both in the medical community and in everyday life. Wearing masks in routine daily settings has become an essential means of self-protection to prevent the spread of the virus [2]. In Korea, COVID-19 patients and non-infected people mainly wear KF94 masks (South Korean government’s standards), while medical staff wear N95 masks in isolation wards. Therefore, complications caused by the use of facial masks are commonly observed in the general population. According to a study of 2136 people surveyed about the discomfort of regular mask wearing during the COVID-19 pandemic, the types of discomfort reported by members of the general population included breathing difficulties, headaches, ear pain, mask-related infections, and skin irritation. The most common complication was difficulty breathing (reported by 60% of participants), followed by ear pain (22%) and itchy skin (16%) [3].
Pressure injuries cause damage to the skin and soft tissues when intense and continuous pressure is applied, which can result from wearing protective equipment. Generally, surgical, N95, and KF94 masks are disposable masks that are available in the Korean market. N95 masks are known to be the most effective protective equipment for preventing respiratory virus infections. However, skin injuries due to prolonged pressure on the skin while wearing an N95 mask for extended periods of time, including during long hospitalizations, have been studied since the outbreak of COVID-19 [2,4]. A study conducted among medical staff who wore masks or goggles found that the nose bridge and cheeks were the most common anatomical locations of complications, accounting for 59.65%, although protective equipment also generated pressure on areas including the ears, forehead, zygoma, mandible, and eyebrow arch [5,6]. Most disposable non-N95 masks available in the market have a strap structure that can apply continuous physical force to the retroauricular region, potentially causing retroauricular or root pressure injury in the helix area.
In plastic surgery, skin grafting is a good reconstructive option to cover skin defects caused by head and neck cancers or trauma. The decrease in outdoor activity due to the COVID-19 pandemic has reduced the rate of facial trauma, but the incidence of facial skin cancer is steadily increasing [7,8]. Common donor sites of full-thickness skin grafts (FTSGs) for head and neck reconstruction are the preauricular skin, retroauricular skin, the clavicle, and inner upper-arm regions [9]. Among these options, the most preferred donor site is the retroauricular donor site, the cosmetic advantages of which include hiding scars and color-matching around the defect [10,11]. The general complications of FTSG donor sites include infection, pain, hypertrophic scarring, and itching [12]. However, few studies have investigated whether the retroauricular FTSG donor site has a functional effect on daily life. Starting in 2020, when widespread and habitual mask wearing became common due to the COVID-19 pandemic, the authors empirically observed the occurrence of complications caused by prolonged mask wearing. Patients who underwent FTSGs with a retroauricular donor site were retrospectively reviewed in this study, and the type and incidence of complications related to mask wearing were analyzed. Even after the COVID-19 pandemic, we will face situations where masks must be worn frequently in the future. Research on postoperative complications of the donor site associated with mask wearing would help determine whether the retroauricular site is appropriate for selection as the donor site for FTSG in head and neck reconstruction.
METHODS
Design and patients
This study retrospectively investigated complications in patients who underwent skin grafting with a retroauricular donor site at a single institution. In these patients, FTSG was performed to cover skin defects from February 2019 to June 2022, and the left and right sides were not differentiated for the purposes of this study. Although the first case of COVID-19 in Korea occurred in January 2020, this study period extended long after surgery because our aim was to investigate surgical site complications. Patients who underwent surgery before the COVID-19 outbreak were included, and the postoperative period was divided into within 6 months after surgery and more than 6 months after surgery. To investigate discomfort in patients with FTSG performed using a retroauricular donor site during the pandemic, when masks were mandatory in daily life, we excluded acute patients during the dressing and treatment period, and we included follow-up results for patients whose wounds had stabilized during a substantial period of time after stitch removal. This study included 27 patients, most of whom had skin defects due to skin cancer or trauma. The outpatient follow-up took place at least 1 month after the procedure; the patients were interviewed during outpatient visits and were cooperative, mobile, and socially active. Consent for patients who did not visit the outpatient clinic was obtained by telephone, and the complication rate was calculated. A questionnaire was developed containing items from studies related to masks during the COVID-19 pandemic and items based on the symptoms that patients described at the time of hospitalization.
All study participants provided written informed consent for their medical information to be stored in the database and used for research purposes. The study protocol was approved by the Institutional Review Board of Kosin University Gospel Hospital of Korea (KUGH 2022-12-039). All procedures were performed in accordance with the ethical standards of the institutional and national research committee and with the 1964 Helsinki Declaration and its later amendments.
Data sources
To supplement the evidence for investigation, papers were searched from PubMed, Google Scholar, and PRS journals using the following terms: “COVID-19,” “mask-related complication,” “pressure injury,” “retroauricular donor site,” and “retroauricular incision.” The publication period of the studies ranged from 2019 to 2022. Questions on pain, mask sores, deformity, the balance of the mask, itching, and inconvenience in daily life were answered as “yes” or “no,” and additional comments were recorded. To measure the severity of symptoms, scores were measured and compared to those of the unaffected side. The scores were calculated as follows: no complication, 1 point; mild inconvenience, 2 points; moderate complications, 3 points; and severe complications, 4 points.
Surgical technique
The retroauricular region was used as the donor site for FTSG in all patients. At the donor site in the right or left retroauricular region, the appropriate skin size was determined according to the size of the defect with an elliptical design. A mixture of lidocaine with 1:100,000 epinephrine was injected into the margin of the incision. The incision was made using a No. 15 scalpel, undermining was performed, and the skin (determined according to the size of the defect) was collected, including subcutaneous fat. After soaking the collected skin in normal saline, bleeding was controlled using Bovie electrocautery. The collected skin was defatted and fixed using sutures at the donor site. At the donor site, the edge was undermined using small Metzenbaum scissors for approximation. A Penrose silastic drain was inserted to drain the wound discharge. The postoperative wound dressing lasted for approximately a week, and the Penrose silastic drain was removed after an average of 2 days (Fig. 1). Total stitching out of the wound site was performed 1 week after surgery, and the complications that occurred during wound care were recorded.
Data analysis
A questionnaire was administered to 27 patients who underwent FTSG. Categorical variables were analyzed using Fisher exact test. The presence or absence of symptoms according to sex, the type of mask, the location of the donor site, the duration of mask wearing, and the time of operation were analyzed using Fisher exact test. The severity of symptoms was measured using the scores described above. Differences in mean scores were analyzed by the Mann-Whitney test. All statistical analyses were performed using SPSS version 21.0 (IBM Corp.).
RESULTS
According to a literature search, the retroauricular donor site, which has several advantages in head and neck reconstruction, has been studied for postoperative complications and long-term scar evaluation; however, relatively little research has investigated daily discomfort and feasibility in special situations such as the COVID-19 pandemic [13,14]. Since the outbreak of COVID-19, several studies have been published on pressure injuries caused by the use of masks, medical equipment, or prolonged hospitalization. Symptoms such as pressure sores and skin irritation in the forehead, nose, and retroauricular region have been reported following the use of medical equipment, including protective gear [5]. Furthermore, studies that considered continuous wear time found a higher prevalence of symptoms with daily wear times of 3 to 4 hours or more [2].
In the present study, the average age of the patients was 67 years. Twenty-one patients (77.7%) were over 60 years of age and six (22.2%) were under 60 years of age. Most patients had skin cancer, although many of the patients <60 years underwent surgery to cover defects due to trauma. Of the 27 patients, 14 were men and 13 were women, and five patients (three men and two women) reported symptoms associated with mask use.
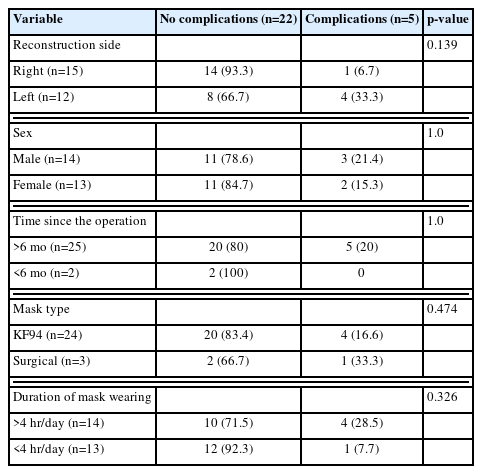
Fourteen patients (51.8%) wore masks continuously for more than 4 hours during the day, of whom four patients (28.5%) had complications. Thirteen patients (48.1%) wore masks for less than 4 hours, of whom only one patient (7.6%) complained of discomfort; however, this difference was not statistically significant (p=0.326) (Table 1).
The most common complications were pain and itching. None of the patients complained of an ear deformity or mask imbalance. All patients, including those with symptoms, stated that they did not experience any discomfort in their daily lives. Five (18.5%) of the 27 patients had complications at the retroauricular donor site, and three of them complained of both pain and itching (Table 2).
To measure the severity of symptoms, the scores were measured and compared with those of the unaffected side. Most patients answered that the score of the donor site was 3 compared with that of the unaffected side. The mean score of patients who complained of pain was 1.48 (p=0.148), and that of patients with discomfort due to itching was 1.40 (p=0.125). The mean scores were low, and no significant differences were obtained (Table 3).
DISCUSSION
The ongoing COVID-19 pandemic has affected countries throughout the world, and the rapid infectivity and pathogenicity of the virus have resulted in major changes in everyday life. Facial masks are the most effective and convenient protective equipment. To prevent infection by droplets, wearing a mask both indoors and outdoors has been compulsory until recently and is still recommended in many countries [1].
As a result of these measures taken to reduce the spread of COVID-19, people are required to wear masks for prolonged periods in their daily lives, leading to local skin pressure injuries. Several studies have identified protective equipment as a risk factor, described the mechanisms of pressure sores related to COVID-19, and argued that local pressure and friction are caused by equipment such as N95 masks and goggles [2,4,6]. Numerous studies have been conducted on medical staff, but studies on patients who underwent surgery in areas prone to pressure injuries are still lacking. Accordingly, the authors conducted a survey to investigate whether wearing a mask could lead to complications in patients who received skin grafts from the retroauricular region.
The average age of the patients who participated in the survey was 67 years, and 77.7% of the patients were >60 years old. Most patients underwent FTSG to cover a defect after wide excision for skin cancer. In general, the intrinsic risk factors for pressure injuries are decreased sensory perception and malnutrition. Although older patients are more likely to have these risk factors, no significant results were obtained [15].
Various studies have reported that continuously wearing protective equipment leads to complications; in particular, it has been widely claimed that continuous compression for more than 4 to 6 hours can cause pressure injuries [2]. In this survey, 51.8% of patients wore masks for more than 4 hours per day, of whom 28.5% answered that they had complications. Meanwhile, 48.1% wore masks for less than 4 hours per day, of whom only one person (7.6%) complained of discomfort. Although this difference was not statistically significant (p=0.326), these findings broadly correspond to the results of a previous study that wearing masks for more than 4 hours was associated with the occurrence of pain and mask pressure scores. None of the patients had undergone prophylactic dressing; they felt moderate discomfort, which did not affect their daily life. Other variables, such as the reconstruction side, gender, time of surgery, and mask type, also did not show significant results.
The most common complaints were pain and itching. The time elapsed since surgery ranged from 2 months to 3 years. Pain or itching when wearing a mask may be due to scar tissue or inflammation in the surgical region [16]; however, patients who felt symptoms when not wearing a mask did not hear. In addition, no patients complained of pain on the contralateral side compared to the surgical site due to numbness caused by temporary damage of the sensory nerve around the incision site [17].
No patients in this study complained of an ear deformity or mask imbalance. Structural deformities can result from excessive skin harvesting to reconstruct a wide defect or from scar contracture; both of these factors can be influenced by the surgeon’s surgical technique or preoperative design. In this study, FTSGs centered on the posterior auricular sulcus were harvested, with a maximum width of 3 cm, height not exceeding the superior auricular root, the highest point at the posterior auricular groove, and a downward extent to the highest point of the posterior ear lobe groove. Therefore, we avoided excessive harvesting that could have caused a deformity.
When harvesting retroauricular skin, the size of the defect is taken into account and the undermining of the flap allows tension-free direct closure of the donor site, which minimizes donor site complications [13]. No hematoma, seroma, flap necrosis, or wound dehiscence was observed in patients during postoperative care, and the mask-related complication rates were comparable to those reported in the general non-operative population (ear pain, 22%; itchy skin 16%) [3]. The complication rate seems to increase slightly with age and daily wearing time; thus, we can say that it is worth being careful with mask wearing in this group of patients, but the results were not statistically significant.
Scar characteristics were only recorded if there were any abnormal findings, and no patients had hypertrophic scars, atrophic scars, or any other abnormal forms of scars. When the scars were assessed, high objective satisfaction was reported. This is similar to the results of a previous paper that objectively quantified satisfaction with scarring at retroauricular donor sites [14].
Since the outbreak of COVID-19, many countries and research institutes have discussed whether social distancing measures or wearing masks in community settings can prevent the spread of this disease [18]. However, there is almost no history of simultaneous mask usage worldwide, and public health stakeholders are wary of the possibility of a similar pandemic situation in the future. During pandemic situations, as exemplified by COVID-19, plastic surgeons can consider the preoperative setting and surgical procedures to prevent the spread of the virus in the context of global health care. It is also necessary to consider whether there are any inconveniences in patients’ lives after surgery [19].
We investigated the incidence of various types of complications at the donor site when wearing a mask in patients who underwent FTSG from the retroauricular region to cover a facial or hand defect and whether these patients experienced inconveniences in daily life. About 18% of patients felt discomfort, but the discomfort did not interfere with their daily life. The use of the retroauricular region as the donor site for FTSG did not affect mask wearing, suggesting that the retroauricular region remains a good choice as a donor site. This study is meaningful in that it reminds patients who have undergone surgical treatment of the need to consider various problems that could arise in the future to avoid feeling uncomfortable in their daily lives.
There are several ways to prevent long-term complications such as pain and itching behind the ear. Pressure damage can be prophylactically reduced with silicone foam dressings and hydrocolloid dressings [2]. However, since it is not cost-effective to use disposable dressing products over prolonged periods, it seems that a similar principle could be applied to commercially available behind-ear protectors or mask loops (Fig. 2). We also suggest the method of wearing masks on the post-antihelical fossa. However, these methods can cause the mask to slip off and affect the fit, potentially interfering with the original purpose of preventing viral infection. In addition, the retroauricular skin surface is reduced after the skin is harvested; thus, mask straps are usually located in the sulcus. Another option is to harvest the retroauricular mastoid skin as the donor site. This avoids the retroauricular sulcus and the harvest can be performed close to the hairline [20]. However, this is a location with relatively visible scars, and it is difficult to harvest a large amount of skin.
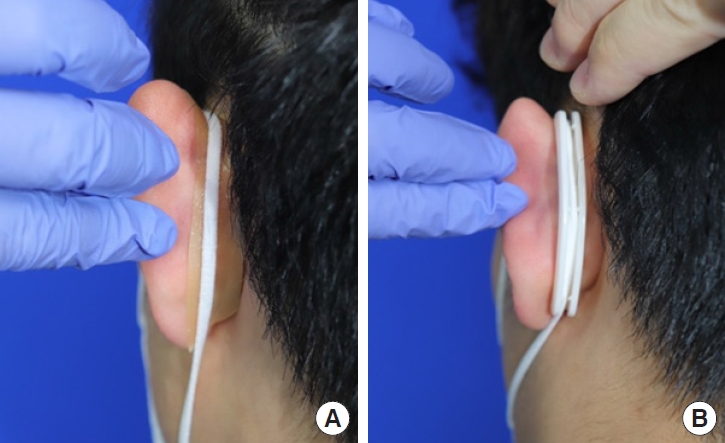
Prophylactic methods to reduce retroauricular pressure. Hydrocolloid dressing by Duoderm Extrathin (A), and a commercially available ear protector (B).
This study has several limitations. The number of patients surveyed was small, and different races and age groups were not considered. The patients did not wear the same masks, and the elasticity of the mask strap may have varied depending on the manufacturer. A more elastic strap has a higher risk of causing pain, and patients may consider replacing masks with highly elastic straps for that reason. However, it should be noted that this was a retrospective study and despite the random choice of mask type, the incidence of surgical site complications on the side of the donor site was comparable to those in the contralateral ear that did not undergo surgery.
The survey’s criteria for complications of continuous mask wearing (more than 4 hours) were based on a systematic review of studies examining pressure injuries related to COVID-19, but we acknowledge that many of the studies were conducted among healthcare workers; thus, it is difficult to know whether masks were worn continuously in the general population. Nonetheless, this study was conducted at the height of the COVID-19 pandemic, and it is reasonable to expect that the patients in the study were very compliant with hygiene practices. In our opinion, it is important to note that none of the patients who wore masks for more than 4 hours a day used aids or changed the way they wore their masks because of pain or discomfort.
In conclusion, the rate of retroauricular donor site-related complications was low, and no complications caused inconvenience in daily life. Therefore, during the COVID-19 pandemic, the use of the retroauricular region as an FTSG donor site remains appropriate.
Abbreviations
COVID-19
coronavirus disease of 2019
FTSG
full-thickness skin graft
Notes
Conflicts of interest
No potential conflict of interest relevant to this article was reported.
Ethical approval
The study was conducted in accordance with the Declaration of Helsinki and approved by the Institutional Review Board of Kosin University Gospel Hospital of Korea (KUGH 2022-12-039). Informed consent was obtained from all subjects involved in the study.
Patient consent
The patient provided written informed consent for the publication and the use of his images.
Funding
This study was supported by a National Research Foundation of Korea (NRF) grant funded by the Korean government (MSIT) (No. 2020R1G1A1007678).
Author contributions
Conceptualization: Yoon Soo Kim, Jeong Jin Park, Hong Il Kim. Methodology: Jin Hyung Park. Formal analysis: Hyung Suk Yi. Investigation: Jeong Jin Park, Hyung Suk Yi. Resources: Yoon Soo Kim, Hong Il Kim. Data curation: Jeong Jin Park, Yoon Soo Kim. Writing - original draft preparation: Jeong Jin Park, Yoon Soo Kim, Hong Il Kim. Writing - review and editing: Hyung Suk Yi, Hong Il Kim. Visualization: Jin Hyung Park. Supervision: Jin Hyung Park, Yoon Soo Kim. Funding acquisition: Hong Il Kim. All authors have read and agreed to the published version of the manuscript.