1. Urken ML, Moscoso JF, Lawson W, Biller HF. A systematic approach to functional reconstruction of the oral cavity following partial and total glossectomy. Arch Otolaryngol Head Neck Surg 1994;120:589-601.


4. Manrique OJ, Leland HA, Langevin CJ, Wong A, Carey JN, Ciudad P, et al. Optimizing outcomes following total and subtotal tongue reconstruction: a systematic review of the contemporary literature. J Reconstr Microsurg 2017;33:103-11.


6. Absolon KB, Rogers W, Aust JB. Some historical developments of the surgical therapy of tongue cancer from the seventeenth to the nineteenth century. Am J Surg 1962;104:686-91.


7. Gilbert RW. Reconstruction of the oral cavity; past, present and future. Oral Oncol 2020;108:104683.


8. Ariyan S. The pectoralis major myocutaneous flap: a versatile flap for reconstruction in the head and neck. Plast Reconstr Surg 1979;63:73-81.


9. Sieczka EM, Weber RV. Climbing the reconstructive ladder in the head and neck. Mo Med 2006;103:265-9.

11. Ye W, Hu J, Zhu H, Zhang Z. Tongue reconstruction with tongue base island advancement flap. J Craniofac Surg 2013;24:996-8.


12. Nueangkhota P, Liang YJ, Zheng GS, Su YX, Yang WF, Liao GQ. Reconstruction of tongue defects with the contralateral nasolabial island flap. J Oral Maxillofac Surg 2016;74:851-9.


13. Joseph ST, Naveen BS, Mohan TM. Islanded facial artery musculomucosal flap for tongue reconstruction. Int J Oral Maxillofac Surg 2017;46:453-5.


14. Sittitrai P, Reunmakkaew D, Srivanitchapoom C. Submental island flap versus radial forearm free flap for oral tongue reconstruction: a comparison of complications and functional outcomes. J Laryngol Otol 2019;133:413-8.


15. Bokhari WA, Wang SJ. Tongue reconstruction: recent advances. Curr Opin Otolaryngol Head Neck Surg 2007;15:202-7.


17. Hanasono MM, Matros E, Disa JJ. Important aspects of head and neck reconstruction. Plast Reconstr Surg 2014;134:968e-980e.


18. Hartl DM, Dauchy S, Escande C, Bretagne E, Janot F, Kolb F. Quality of life after free-flap tongue reconstruction. J Laryngol Otol 2009;123:550-4.


19. Chen WL, Yang ZH, Li JS, Huang ZQ. Reconstruction of the tongue using an extended vertical lower trapezius island myocutaneous flap after removal of advanced tongue cancer. Br J Oral Maxillofac Surg 2008;46:379-82.


20. Engel H, Huang JJ, Lin CY, Lam W, Kao HK, Gazyakan E, et al. A strategic approach for tongue reconstruction to achieve predictable and improved functional and aesthetic outcomes. Plast Reconstr Surg 2010;126:1967-77.


22. de Vicente JC, de Villalain L, Torre A, Pena I. Microvascular free tissue transfer for tongue reconstruction after hemiglossectomy: a functional assessment of radial forearm versus anterolateral thigh flap. J Oral Maxillofac Surg 2008;66:2270-5.


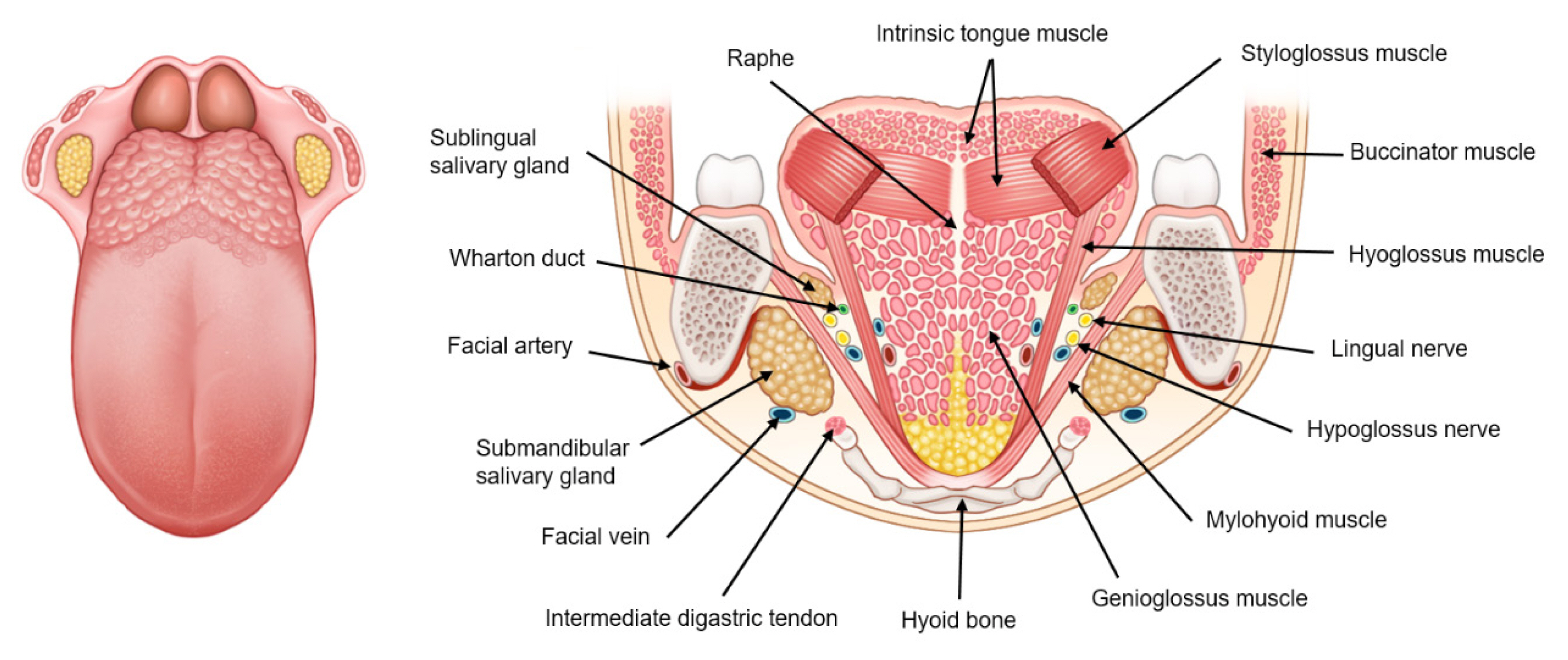
24. Baas M, Duraku LS, Corten EM, Mureau MA. A systematic review on the sensory reinnervation of free flaps for tongue reconstruction: does improved sensibility imply functional benefits? J Plast Reconstr Aesthet Surg 2015;68:1025-35.


26. Liao G, Su Y, Zhang J, Hou J, Chen Y, Li M. Reconstruction of the tongue with reinnervated rectus abdominis musculoperitoneal flaps after hemiglossectomy. J Laryngol Otol 2006;120:205-13.


27. Haughey BH, Fredrickson JM. The latissimus dorsi donor site: current use in head and neck reconstruction. Arch Otolaryngol Head Neck Surg 1991;117:1129-34.


28. Park H, Park JS, Jeong WS, Choi JW. Dynamic hemitongue defect reconstruction with functional gracilis muscle free transfer. Ann Plast Surg 2021;86:308-16.


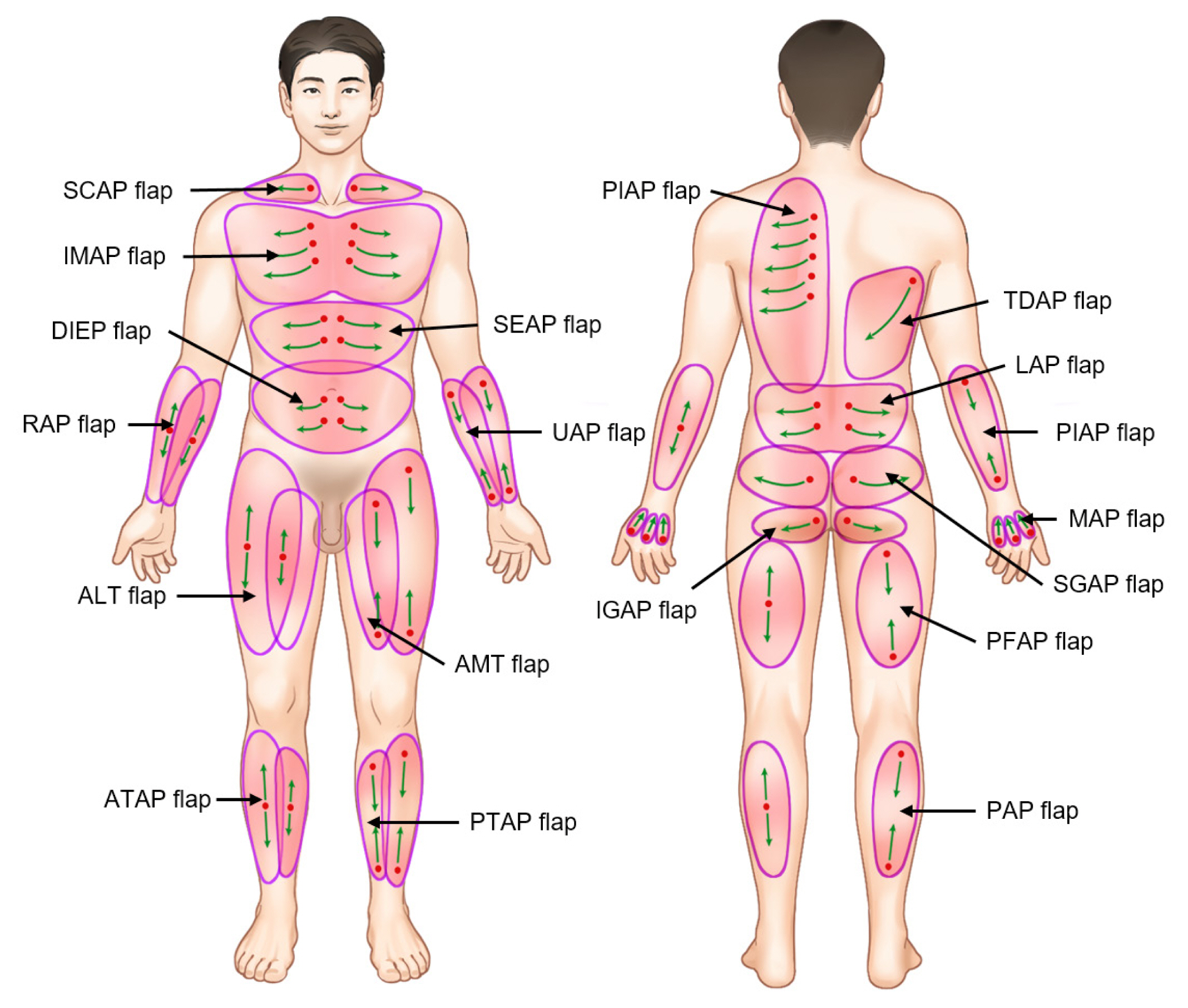
29. Pribaz JJ, Chan RK. Where do perforator flaps fit in our armamentarium? Clin Plast Surg 2010;37:571-9.


30. Choi JW. Perforator flaps in head and neck reconstruction: a review article of “the current state of the art”. Otorinolaringologia 2014;64:13-21.
32. Wolff KD, Rau A, Kolk A. Perforator flaps from the lower leg for intraoral reconstruction: experience of 131 flaps. J Craniomaxillofac Surg 2018;46:338-45.


34. Ali RS, Bluebond-Langner R, Rodriguez ED, Cheng MH. The versatility of the anterolateral thigh flap. Plast Reconstr Surg 2009;124(6 Suppl):e395-407.


35. Zhang PP, Meng L, Shen J, Liu H, Zhang J, Xiang X, et al. Free radial forearm flap and anterolateral thigh flap for reconstruction of hemiglossectomy defects: a comparison of quality of life. J Craniomaxillofac Surg 2018;46:2157-63.


36. Choi JW, Kim YC, Oh TS, Koh KS, Jeong WS. The versatile use of revisited de-epithelialization concept in superficial circumflex iliac and anterolateral thigh perforator free flap for head and neck reconstructions. J Craniomaxillofac Surg 2017;45:872-80.


37. Choi JW, Nam SY, Choi SH, Roh JL, Kim SY, Hong JP. Applications of medial sural perforator free flap for head and neck reconstructions. J Reconstr Microsurg 2013;29:437-42.


38. Largo RD, Bhadkamkar MA, Asaad M, Chu CK, Garvey PB, Butler CE, et al. The profunda artery perforator flap: a versatile option for head and neck reconstruction. Plast Reconstr Surg 2021;147:1401-12.


39. Ferrari M, Sahovaler A, Chan HH, Nicolai P, Irish JC, Gilbert RW. Scapular tip-thoracodorsal artery perforator free flap for total/subtotal glossectomy defects: case series and conformance study. Oral Oncol 2020;105:104660.


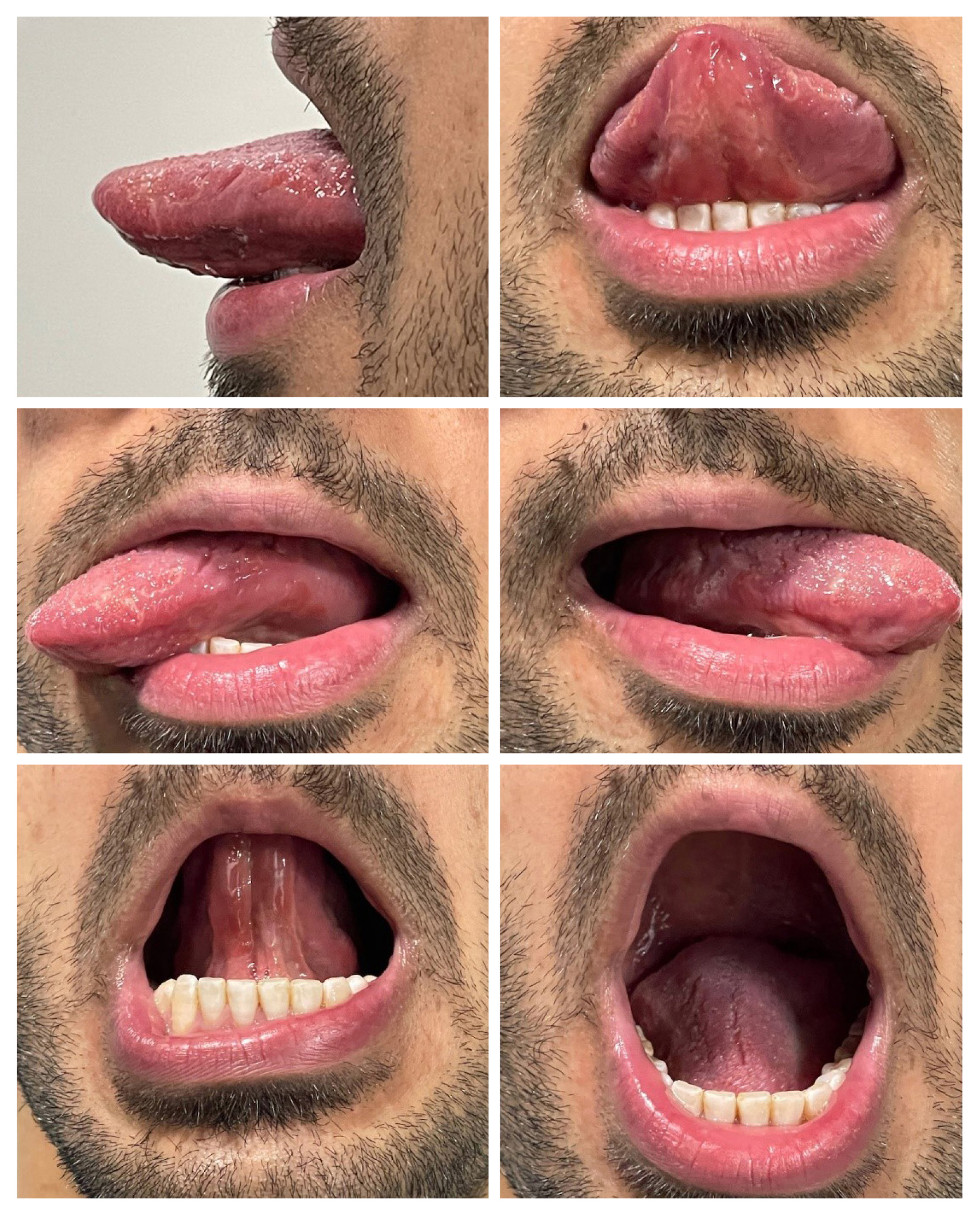
42. Chepeha DB, Spector ME, Chinn SB, Casper KA, Chanowski EJ, Moyer JS, et al. Hemiglossectomy tongue reconstruction: modeling of elevation, protrusion, and functional outcome using receiver operator characteristic curve. Head Neck 2016;38:1066-73.


43. Matsui Y, Ohno K, Yamashita Y, Takahashi K. Factors influencing postoperative speech function of tongue cancer patients following reconstruction with fasciocutaneous/myocutaneous flaps: a multicenter study. Int J Oral Maxillofac Surg 2007;36:601-9.


44. Uwiera T, Seikaly H, Rieger J, Chau J, Harris JR. Functional outcomes after hemiglossectomy and reconstruction with a bilobed radial forearm free flap. J Otolaryngol 2004;33:356-9.


50. Urken ML, Weinberg H, Vickery C, Buchbinder D, Lawson W, Biller HF. Oromandibular reconstruction using microvascular composite free flaps: report of 71 cases and a new classification scheme for bony, soft-tissue, and neurologic defects. Arch Otolaryngol Head Neck Surg 1991;117:733-44.


53. de Almeida JR, Park RC, Villanueva NL, Miles BA, Teng MS, Genden EM. Reconstructive algorithm and classification system for transoral oropharyngeal defects. Head Neck 2014;36:934-41.


54. Kimata Y, Sakuraba M, Hishinuma S, Ebihara S, Hayashi R, Asakage T, et al. Analysis of the relations between the shape of the reconstructed tongue and postoperative functions after subtotal or total glossectomy. Laryngoscope 2003;113:905-9.


55. Yun IS, Lee DW, Lee WJ, Lew DH, Choi EC, Rah DK. Correlation of neotongue volume changes with functional outcomes after long-term follow-up of total glossectomy. J Craniofac Surg 2010;21:111-6.


57. Tarsitano A, Battaglia S, Cipriani R, Marchetti C. Microvascular reconstruction of the tongue using a free anterolateral thigh flap: three-dimensional evaluation of volume loss after radiotherapy. J Craniomaxillofac Surg 2016;44:1287-91.


58. Bittermann G, Thonissen P, Poxleitner P, Zimmerer R, Vach K, Metzger MC. Microvascular transplants in head and neck reconstruction: 3D evaluation of volume loss. J Craniomaxillofac Surg 2015;43:1319-24.


61. Yamamoto Y, Sugihara T, Furuta Y, Fukuda S. Functional reconstruction of the tongue and deglutition muscles following extensive resection of tongue cancer. Plast Reconstr Surg 1998;102:993-1000.


62. Riva G, Sapino S, Ravera M, Elia G, Pecorari G. Long-term functional outcomes and quality of life after partial glossectomy for T2 squamous cell carcinomas. Braz J Otorhinolaryngol. 2021 Jul 30 [Epub].
https://doi.org/10.1016/j.bjorl.2021.06.009.

63. Dziegielewski PT, Ho ML, Rieger J, Singh P, Langille M, Harris JR, et al. Total glossectomy with laryngeal preservation and free flap reconstruction: objective functional outcomes and systematic review of the literature. Laryngoscope 2013;123:140-5.


64. Matsui Y, Shirota T, Yamashita Y, Ohno K. Analyses of speech intelligibility in patients after glossectomy and reconstruction with fasciocutaneous/myocutaneous flaps. Int J Oral Maxillofac Surg 2009;38:339-45.


65. Sun J, Weng Y, Li J, Wang G, Zhang Z. Analysis of determinants on speech function after glossectomy. J Oral Maxillofac Surg 2007;65:1944-50.


66. Lam L, Samman N. Speech and swallowing following tongue cancer surgery and free flap reconstruction: a systematic review. Oral Oncol 2013;49:507-24.


67. Shin YS, Koh YW, Kim SH, Jeong JH, Ahn S, Hong HJ, et al. Radiotherapy deteriorates postoperative functional outcome after partial glossectomy with free flap reconstruction. J Oral Maxillofac Surg 2012;70:216-20.


68. Yi CR, Jeong WS, Oh TS, Koh KS, Choi JW. Analysis of speech and functional outcomes in tongue reconstruction after hemiglossectomy. J Reconstr Microsurg 2020;36:507-13.


69. Ravindra A, Nayak DR, Devaraja K, Matthew NM, Tiwari S. Functional outcomes after surgical resection of tongue cancer; a comparative study between primary closure, secondary intention healing and flap reconstruction. Indian J Otolaryngol Head Neck Surg. 2022 Jan 5 [Epub].
https://doi.org/10.1007/s12070-021-03038-1.

72. Choi JW, Lee MY, Oh TS. The application of multilobed flap designs for anatomic and functional oropharyngeal reconstructions. J Craniofac Surg 2013;24:2091-7.


73. Brown L, Rieger JM, Harris J, Seikaly H. A longitudinal study of functional outcomes after surgical resection and microvascular reconstruction for oral cancer: tongue mobility and swallowing function. J Oral Maxillofac Surg 2010;68:2690-700.


74. Rieger JM, Zalmanowitz JG, Li SY, Sytsanko A, Harris J, Williams D, et al. Functional outcomes after surgical reconstruction of the base of tongue using the radial forearm free flap in patients with oropharyngeal carcinoma. Head Neck 2007;29:1024-32.


75. Yanai C, Kikutani T, Adachi M, Thoren H, Suzuki M, Iizuka T. Functional outcome after total and subtotal glossectomy with free flap reconstruction. Head Neck 2008;30:909-18.


76. Fujimoto Y, Matsuura H, Kawabata K, Takahashi K, Tayama N. Assessment of Swallowing Ability Scale for oral and oropharyngeal cancer patients. Nihon Jibiinkoka Gakkai Kaiho 1997;100:1401-7.


77. Pedersen A, Wilson J, McColl E, Carding P, Patterson J. Swallowing outcome measures in head and neck cancer: how do they compare? Oral Oncol 2016;52:104-8.


78. Thankappan K, Kuriakose MA, Chatni SS, Sharan R, Trivedi NP, Vijayaraghavan S, et al. Lateral arm free flap for oral tongue reconstruction: an analysis of surgical details, morbidity, and functional and aesthetic outcome. Ann Plast Surg 2011;66:261-6.