|
 |
- Search
| Arch Craniofac Surg > Volume 24(4); 2023 > Article |
|
Abstract
An epidermal cyst, also known as an epidermoid cyst or epidermal inclusion cyst, is the most prevalent type of cutaneous cyst. This noncancerous lesion can appear anywhere on the body, typically presenting as an asymptomatic dermal nodule with a visible central punctum. In the case presented herein, an epidermal cyst with uncommon features was misdiagnosed as a lymphatic malformation based on preoperative magnetic resonance imaging (MRI). A 61-year-old man came to us with a swollen left cheek that had been present for 11 months. The preoperative MRI revealed a 3 ├Ś 3.8 ├Ś 4.6 cm lobulated cystic lesion with thin rim enhancement in the left masticator space. The initial differential diagnosis pointed toward a lymphatic malformation. We proceeded with surgical excision of the lesion via an intraoral approach, and the specimen was sent to the pathology department. The pathological diagnosis revealed a ruptured epidermal cyst, indicating that the initial diagnosis of a lymphatic malformation based on preoperative MRI was incorrect. Epidermal cysts located under the muscle with no visible central punctum are uncommon, but should be considered if a patient presents with facial swelling.
An epidermal cyst, also known as an epidermoid cyst or epidermal inclusion cyst, is the most prevalent type of cutaneous cyst. This non-cancerous lesion can appear anywhere on the body, typically manifesting as an asymptomatic dermal nodule with a visible central punctum. The distribution of these lesions on the face is as follows: 20.8% appear on the cheek, 12.7% in the periauricular area, 10.9% in the periorbital area, 6.0% in the frontal area, 5.6% in the mental area, 3.7% in the perioral area, 2.8% in the nasal area, and 2.5% in the temporal area [1]. The lesions can be solitary or multiple [2]. In the case presented herein, an intramuscular epidermal cyst with an uncommon feature was misdiagnosed as a lymphatic malformation based on preoperative magnetic resonance imaging (MRI).
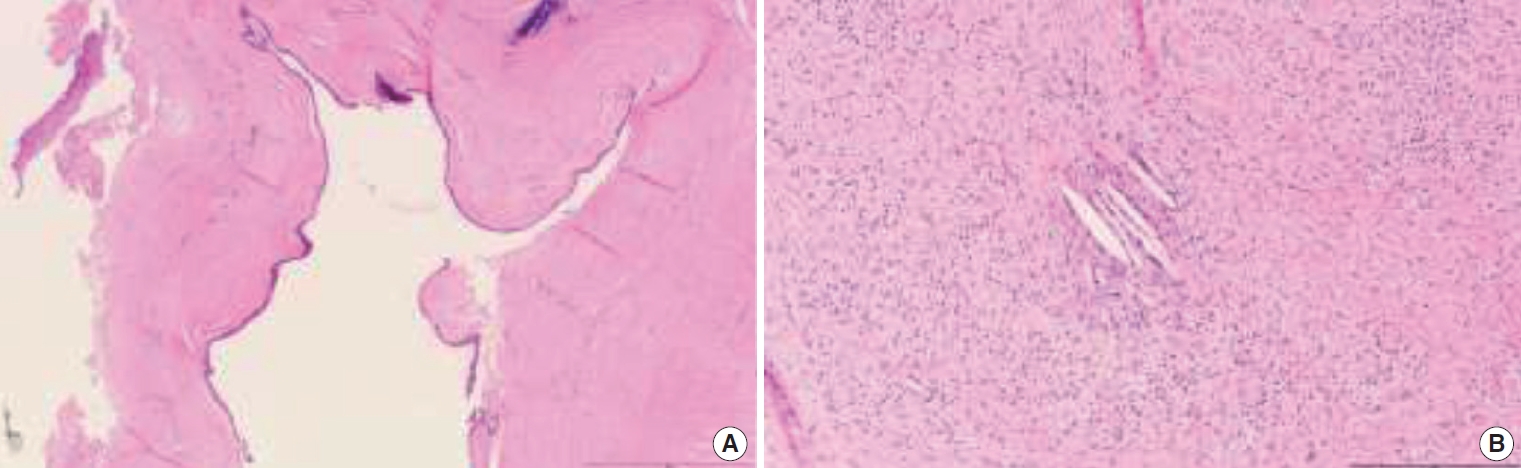
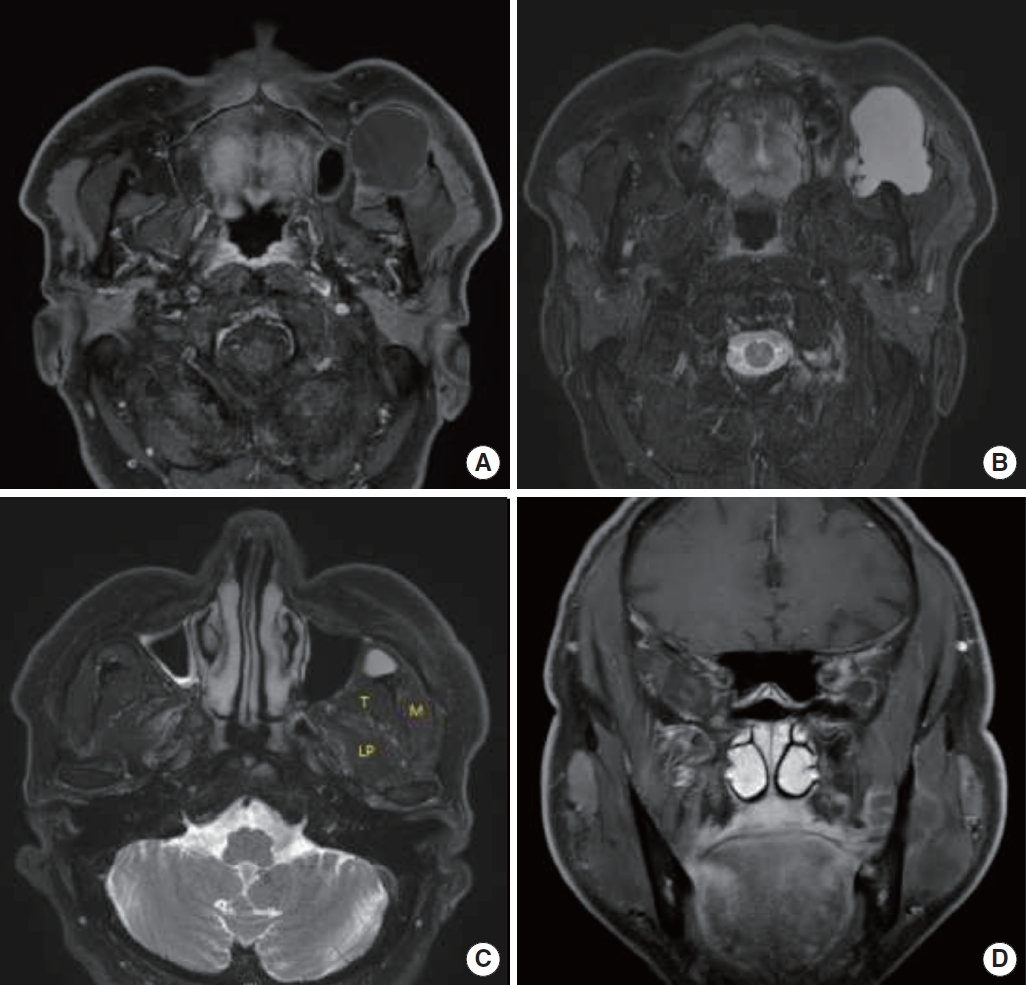
A 61-year-old man presented with a swollen left cheek that had persisted for 11 months. He exhibited left buccal mucosa swelling. He had no prior history of trauma or surgical procedures. A preoperative MRI revealed a lobulated cystic lesion, measuring 3 ├Ś 3.8 ├Ś 4.6 cm, with thin rim enhancement. This lesion was situated in the left masticator space and extended along the anterior border of the mandibular ramus. The lesion exhibited low signal intensity on T1-weighted imaging and high signal intensity on T2-weighted imaging (Fig. 1). Due to a lobulated cystic lesion, the differential diagnosis pointed toward a lymphatic malformation. To facilitate access to the tumor, the lesion was excised intraorally under general anesthesia, through an incision along the anterior border of the mandibular ramus. Upon gross examination, the lesion was found to have a thin-walled capsule filled with a cheesy white material (Fig. 2). A histopathological examination of the specimen revealed a cystic lining composed of stratified squamous epithelium, a foreign body giant cell reaction, histiocytic aggregation around the epidermal cyst, and keratin entrapment within the connective tissue (Fig. 3). The pathological diagnosis confirmed a ruptured epidermal cyst.
Epidermal cysts are benign pathologies that can occur anywhere on the body. Approximately 7% of these tumors are found in the head and neck, and the oral cavity accounts for only 1.6% of cases [3]. Dermoid and epidermal cysts in the mouth are particularly uncommon, accounting for < 0.01% of all oral cysts. Most of these occur in the sublingual region; however, there are limited case reports of their occurrence at other sites [4]. Epidermal cysts are believed to originate from the entrapment of epithelial remnants during the midline closure of the bilateral first and second branchial arches [5] or traumatic implantation of the epithelium. These cysts can occur in any age group, but they are most commonly found in individuals between the ages of 15 and 35 years, with a male predilection [6]. In this case, a 61-year-old man had an idiopathic epidermal cyst. He had no history of trauma or a surgical procedure.
Most epidermal cysts are confined to the skin and subcutaneous tissues. There have been only a handful of reported cases of intramuscular epidermal cysts [7-9]. To the best of our knowledge, there have been no previous reports of facial intramuscular epidermal cysts.
Shibata et al. [10] described the MRI features of five cases of epidermal cysts in the extremities. They reported that epidermal cysts had high signal intensity on T2-weighted imaging. Gadolinium-enhanced MRI showed central non-enhancement and peripheral thin rim enhancement. Certain solid tumors, such as neurogenic tumors, nodular fasciitis, myxoid tumors, and dermatofibrosarcoma protuberans, sometimes displayed high signal intensity on T2-weighted imaging and mimicked cystic masses. However, contrast-enhanced MRI showed variable central enhancement within these masses, a finding that is especially helpful for distinguishing solid tumors from epidermal cysts [11].
In cases of lymphatic malformation, MRI scans typically reveal the masses as having low signal intensity on T1-weighted imaging and high signal intensity on T2-weighted imaging. This suggests a fluid content, and the masses often have regular margins, thin walls, and internal septa. After the administration of gadolinium, only the walls and the internal septa display an increased signal intensity on T1-weighted imaging, with no internal contrast enhancement observed [12]. Generally, uni-lobulated lesions are more commonly associated with epidermal cysts, while lymphatic malformations tend to be multi-lobulated [13]. In this case, MRI showed low signal intensity on T1-weighted imaging, high signal intensity on T2-weighted imaging, and thin rim enhancement. Moreover, in the coronal view of T1-weighted imaging, the lesion appeared multi-lobulated in some areas (Fig. 1D). Therefore, it was challenging to differentiate between an epidermal cyst and a lymphatic malformation using MRI.
Histologically, lymphatic malformations are primarily composed of vascular spaces filled with protein-rich and eosinophilic fluid. These spaces are lined by a flattened, single layer of endothelium. The walls of these vessels can vary in thickness and may contain abnormal smooth muscle tissue. Collections of lymphocytes are also observed throughout the connective tissue [14,15]. In this particular case, the histopathology of the specimen revealed a cystic lining made up of stratified squamous epithelium. There was also a foreign body giant cell reaction, histiocytic aggregation around an epidermal cyst, and keratin entrapment in the connective tissue. These findings are indicative of an epidermal cyst. Epidermoid, dermoid, and teratoid cysts are cystic malformations that are lined with squamous epithelium. They are classified based on their lining and contents. Epidermoid cysts are lined with simple squamous epithelium, dermoid cysts have skin adnexa within the cystic wall, and teratoid cysts contain other tissues, such as muscle, cartilage, and bone [16].
Odontogenic keratocysts should also be differentiated within the buccal mucosa. This condition presents as a uni-lobular osteolytic lesion with minimal septa, growing along the length of the bone with minimal buccolingual expansion. Various authors have reported that most odontogenic keratocysts exhibit intermediate or high signal intensity on T1-weighted imaging, and a heterogeneous signal intensity (ranging from low to high) on T2-weighted imaging [17]. Histologically, these cells exhibit a characteristic palisading pattern of cuboidal basal cells, along with parakeratinization resulting in a corrugated surface. Additionally, they do not possess rete ridges and frequently display separation from their basement membrane [18].
Treatment involves complete surgical removal without rupture, as leakage of cystic contents onto the underlying fibrovascular structures can lead to postoperative inflammation [19]. There was noticeable swelling in the left buccal mucosa. The lesion was excised intraorally under general anesthesia through an incision made along the anterior border of the mandibular ramus. The primary benefits of the intraoral approach include easy access to the tumor and an unnoticeable postoperative scar. However, this method may not provide sufficient exposure for optimal tumor resection and identification of nearby nerves [20].
In this instance, the epidermal cyst was incorrectly identified as a lymphatic malformation on preoperative MRI. While epidermal cysts in the masticator space are rare, they should be considered if a patient exhibits facial swelling.
Notes
Ethical approval
The report was approved by the Institutional Review Board of Wonju Severance Christian Hospital (IRB No. CR323320).
Fig.┬Ā1.
A 61-year-old man had a 3├Ś3.8├Ś4.6 cm cystic lesion, which was located in the left masticator space on preoperative magnetic resonance imaging. (A) T1-weighted image (axial view). (B) T2-weighted image with fat suppression (axial view). (C) T2-weighted image with fat suppression (axial view), showing masseter (M), temporalis (T), and lateral pterygoid (LP) muscles. (D) A multi-lobulated cystic lesion was noticed (coronal view).
REFERENCES
1. Kim CS, Na YC, Yun CS, Huh WH, Lim BR. Epidermoid cyst: a single-center review of 432 cases. Arch Craniofac Surg 2020;21:171-5.




2. Baykal C, Yazganoglu KD. Clinical atlas of skin tumors. Springer; 2014.
3. Koca H, Seckin T, Sipahi A, Kazanc A. Epidermoid cyst in the floor of the mouth: report of a case. Quintessence Int 2007;38:473-7.

4. Rajayogeswaran V, Eveson JW. Epidermoid cyst of the buccal mucosa. Oral Surg Oral Med Oral Pathol 1989;67:181-4.


5. Kandogan T, Koc M, Vardar E, Selek E, Sezgin O. Sublingual epidermoid cyst: a case report. J Med Case Rep 2007;1:87.




6. Hemaraju N, Nanda SK, Medikeri SB. Sub-lingual dermoid cyst. Indian J Otolaryngol Head Neck Surg 2004;56:218-20.




7. Yim Y, Kim NR, Moon SG. Intramuscular epidermal cyst of the buttock: a case report. J Korean Soc Radiol 2018;79:354-8.


8. Chatterjee PK, Chandra AB, Dastidar N. Epidermal cyst in sternomastoid muscle simulating a malignant growth. Indian J Otolaryngol 1976;28:86-7.


9. Bhosle R, Das S, Sarkar AK, Krishnan P. Bilateral intramuscular epidermal cysts in the erector spinae. J Neurosci Rural Pract 2021;12:798-9.



10. Shibata T, Hatori M, Satoh T, Ehara S, Kokubun S. Magnetic resonance imaging features of epidermoid cyst in the extremities. Arch Orthop Trauma Surg 2003;123:239-41.



11. Hong SH, Chung HW, Choi JY, Koh YH, Choi JA, Kang HS. MRI findings of subcutaneous epidermal cysts: emphasis on the presence of rupture. AJR Am J Roentgenol 2006;186:961-6.


12. Romeo V, Maurea S, Mainenti PP, Camera L, Aprea G, Cozzolino I, et al. Correlative imaging of cystic lymphangiomas: ultrasound, CT and MRI comparison. Acta Radiol Open 2015;4:2047981614564911.




13. Reiter MJ, Schwope RB, Bui-Mansfield LT, Lisanti CJ, Glasgow SC. Surgical management of retrorectal lesions: what the radiologist needs to know. AJR Am J Roentgenol 2015;204:386-95.


14. Elluru RG, Balakrishnan K, Padua HM. Lymphatic malformations: diagnosis and management. Semin Pediatr Surg 2014;23:178-85.


15. Smith SN. Lymphatic malformations: an overview of pathology, imaging, and treatment. J Radiol Nurs 2019;38:168-73.

16. Jham BC, Duraes GV, Jham AC, Santos CR. Epidermoid cyst of the floor of the mouth: a case report. J Can Dent Assoc 2007;73:525-8.

17. Borghesi A, Nardi C, Giannitto C, Tironi A, Maroldi R, Di Bartolomeo F, et al. Odontogenic keratocyst: imaging features of a benign lesion with an aggressive behaviour. Insights Imaging 2018;9:883-97.




18. Yamamoto K, Matsusue Y, Kurihara M, Takahashi Y, Kirita T. A keratocyst in the buccal mucosa with the features of keratocystic odontogenic tumor. Open Dent J 2013;7:152-6.




19. Shear M, Speight PM. Cysts of the oral and maxillofacial regions. 4th ed. Blackwell Munksgaard; 2007.
- TOOLS
-
METRICS

-
- 1 Crossref
- Scopus
- 1,498 View
- 42 Download
- Related articles in ACFS
-
Intraosseous vascular malformation of the skull: a case report and literature review ;0()
Solitary fibrofolliculoma on the nasal septum: a case report2023 June;24(3)
Primary non-Hodgkin lymphoma of the parotid gland: a case report2022 June;23(3)