Delayed treatment of traumatic eyeball dislocation into the maxillary sinus and treatment algorithm: a case report and literature review
Article information
Abstract
Orbital floor fractures are commonly encountered, but the dislocation of the eyeball into the maxillary sinus is relatively rare. When it does occur, globe dislocation can have serious consequences, including vision loss, enucleation, and orbito-ocular deformity. Immediate surgical intervention is typically attempted when possible. However, severe comorbidities and poor general health can delay necessary surgery. In this report, we present the surgical outcomes of a 70-year-old woman who received delayed treatment for traumatic eyeball dislocation into the maxillary sinus due to a subarachnoid hemorrhage and hemopneumothorax. Additionally, we propose a treatment algorithm based on our clinical experience and a review of the literature.
INTRODUCTION
Blunt facial trauma can lead to fractures of the orbital walls. The mechanisms behind these fractures include increased hydraulic pressure within the orbit and mechanical buckling from external forces [1]. Although the eyeball is largely shielded from injury by numerous suspensory structures, traumatic dislocation of the globe into the maxillary sinus is still possible, albeit rare [2-4]. However, in cases of blunt trauma with extremely high energy, the eyeball can be displaced into the maxillary sinus. This severe displacement may result in permanent vision loss, necessitate enucleation of the eyeball, and lead to postenucleation socket syndrome (PESS), characterized by orbitoocular deformity [2-7].
Although a range of surgical treatments have been introduced to address globe dislocation into the maxillary sinus, debate continues regarding the optimal timing for repositioning the eyeball and reconstructing the orbital floor [3]. Additionally, there is scant information on the outcomes of delayed surgical intervention resulting from a patient’s poor general condition and associated cerebro-pulmonary injuries.
Herein, we present a case involving an unavoidable delay in the treatment of traumatic eyeball dislocation into the maxillary sinus and propose a treatment algorithm based on a review of the literature.
CASE REPORT
A 70-year-old woman presented with multiple injuries resulting from blunt trauma inflicted by cows’ hooves. Upon arrival at the emergency room, the unconscious patient was promptly intubated.
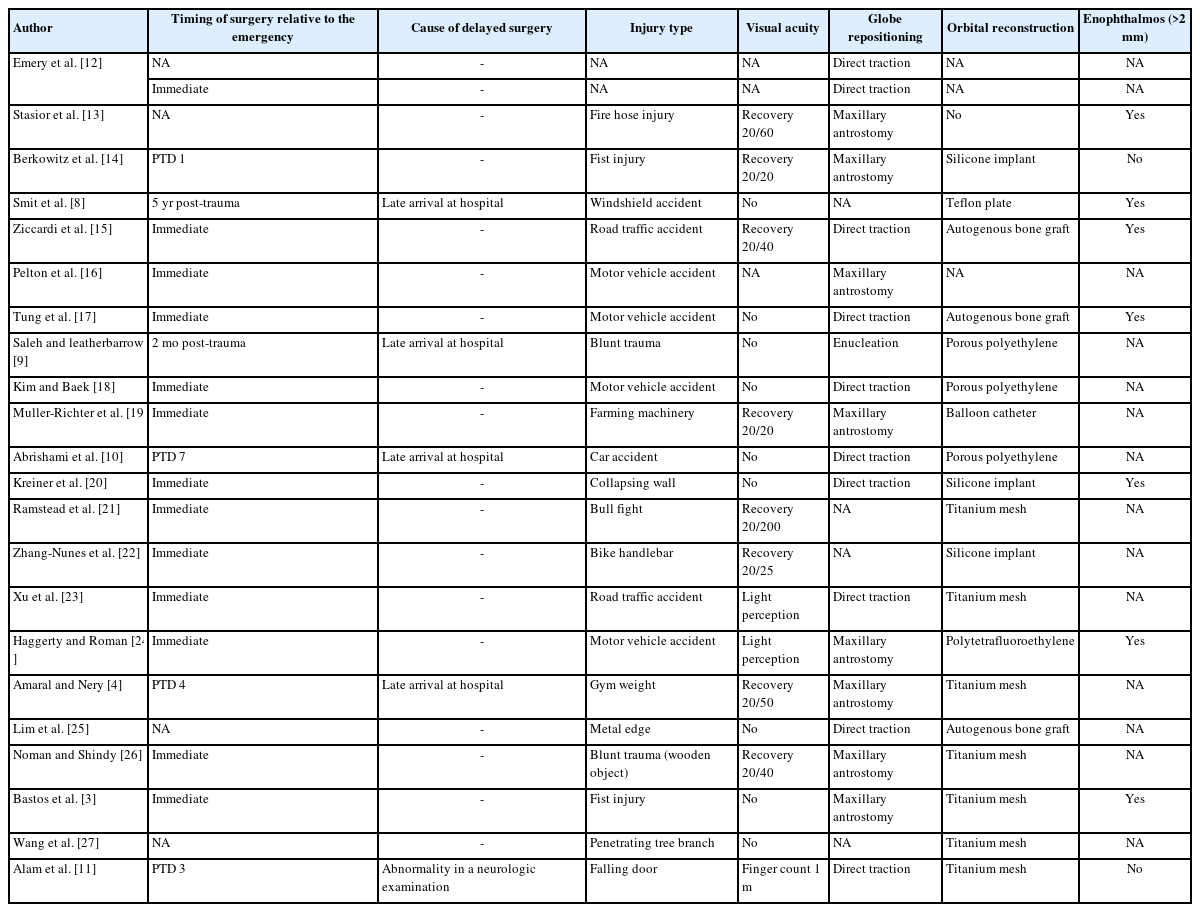
Upon physical examination, significant periorbital ecchymosis was noted, and the right eyeball could not be visualized. Brain and chest computed tomography (CT) showed a subarachnoid hemorrhage (SAH) and multiple rib fractures resulting in a flail chest, as well as hemopneumothorax (Fig. 1A and B). A CT scan of the facial bones revealed a large orbital floor fracture with the dislocation of the eyeball into the right maxillary sinus. This was accompanied by substantial retrobulbar hemorrhage and complete obliteration of the extraocular muscles (EOMs) and optic nerve (Fig. 1C).
Computed tomography (CT) scans of traumatic globe dislocation. (A) A brain CT image shows subarachnoid hemorrhage (red arrow). (B) A chest CT image shows the presence of hemopneumothorax (blue arrow). (C) Overt globe dislocation into the maxillary sinus is shown on facial CT with enhancement. Intact blood flow, including a patent ophthalmic artery (yellow arrow) and ciliary artery (purple arrow), into the orbit and eyeball is identified.
Emergency surgery was mandatory for repositioning the eyeball and preserving visual acuity. However, before the surgery, the patient required intensive care unit (ICU) management for SAH and flail chest with hemopneumothorax. To prevent exacerbated inflammation, infection, and sympathetic ophthalmia in the severely injured eyeball and orbit, conservative treatment was performed. This included fluoroquinolone eyedrops (Ofloxacin; Santen Pharm.) and 0.1% fluorometholone eyedrops (Flumetholon; Santen Pharm.). Additionally, a gentle pressure patch bandage was applied to lightly close the affected eye. To protect the traumatized connective tissue in the orbit and encourage healing, alternating antiseptic and 0.9% saline irrigations were performed, accompanied by a wet dressing.
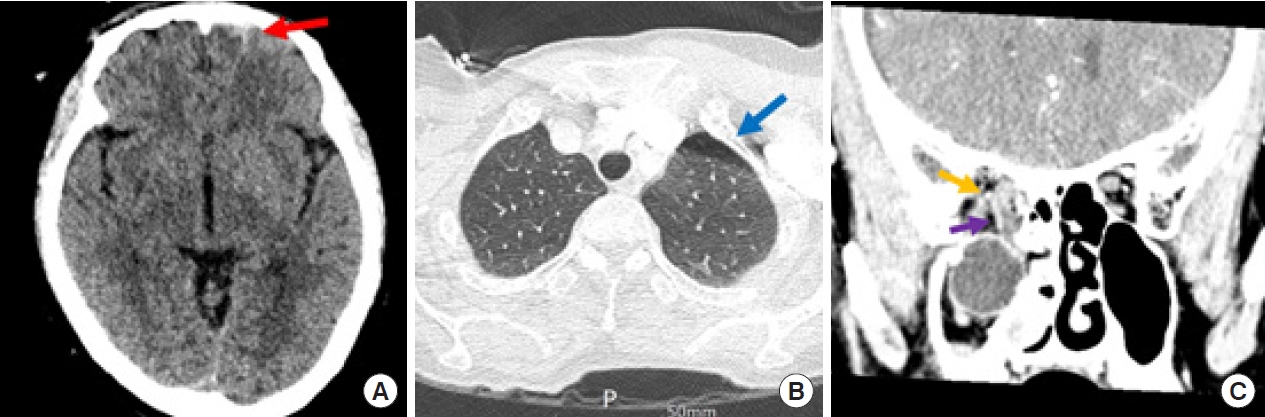
After 2 days of management in the ICU, the patient’s general condition improved. Enhanced facial CT scans showed intact blood flow, including patency of the ophthalmic artery into the orbit and eyeball. Surgical intervention was planned to reposition the dislocated globe. However, the intraoperative findings revealed irreversible ocular injuries, including non-viability of the eyeball and EOMs, along with severance of the optic nerve (Fig. 2). Consequently, an ophthalmologist performed enucleation of the non-viable eyeball and reconstruction of the periorbital microarchitecture.

Intraoperative findings reveal irreversible ocular injuries with a non-viable eyeball and extraocular muscles, as well as permanent damage to the optic nerve.
A porous polyethylene ball implant with a barrier sheet (Medpor; Stryker Instruments) was placed in the orbit. The orbital floor was reconstructed using a biodegradable polymer mesh (Mesh Plate; Inion Ltd.) to minimize the risk of PESS. An ocular prosthesis was then designed and inserted. Nine months postoperatively, a CT scan showed that the right ocular prosthesis was in place without complications (Fig. 3). At the 2-year follow-up, the patient exhibited late enophthalmos on the affected side. Nonetheless, the patient considered the overall surgical outcomes cosmetically acceptable (Fig. 4).
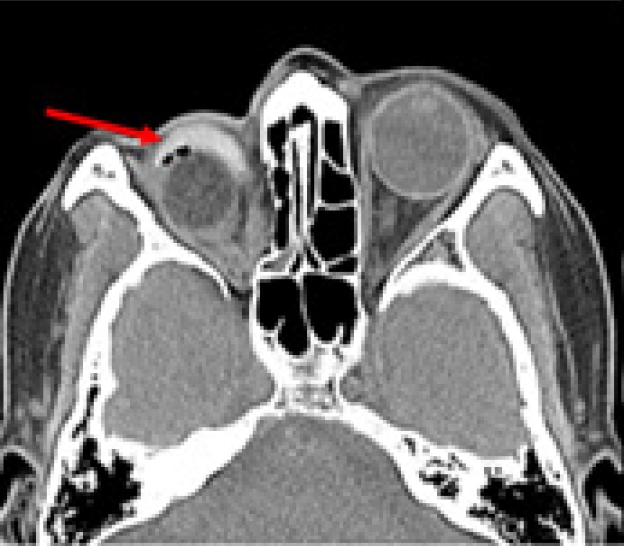
Postoperative computed tomography taken 9 months after surgery. The ocular prosthesis (red arrow) is adequately positioned in the right orbital cavity.
LITERATURE REVIEW
We conducted a review of the relevant literature using the keywords “orbital fracture,” “globe dislocation,” “eyeball displacement,” and “maxillary sinus” in the PubMed, Ovid, and Google Scholar databases. We identified a total of 22 papers related to these keywords [3,4,8-27]. These reports included 23 patients (Table 1). There is no established consensus on the timing and modality of treatment for eyeball displacement into the maxillary sinus. However, due to the increased risk of irreversible vision loss caused by persistent traction on the optic nerve and retinal artery, as well as damage to the microarchitecture of the eyeball, immediate surgical intervention is typically performed in most cases. Of the 23 patients, 21 underwent assessments of postoperative visual acuity. Eleven patients experienced varying degrees of vision recovery, which ranged from light perception or the ability to count fingers to acceptable visual acuity [4,11,19,21-24,26]. Nineteen patients received orbital reconstructions. The methods and materials used for orbital floor reconstruction varied and included a balloon catheter for wall reduction, titanium mesh, silicone sheets, autogenous bone, and polyethylene. Nine patients were evaluated for the occurrence of enophthalmos post-surgery, and seven of them exhibited significant enophthalmos, measuring 2 mm or more [3,8,13,15,17,20,24].
DISCUSSION
Blunt facial trauma can lead to orbital floor fractures. In most cases, even when a large defect with an orbital floor fracture occurs, the surrounding suspensory structures prevent the eyeball from dislocating into the maxillary sinus [1-5]. However, extremely high-energy trauma may cause the complete dislocation of the globe out of the orbit. Once dislocation of the eyeball occurs, serious consequences such as blindness, the necessity for enucleation followed by PESS, and orbito-ocular deformity may arise. Therefore, immediate repositioning of the eyeball is attempted whenever possible, although there is ongoing debate regarding the best supplementary treatments.
Numerous surgical approaches, such as direct globe traction and eyeball repositioning through maxillary antrostomy, have been introduced [3,4]. However, there is limited information available regarding delayed surgical outcomes in patients with poor general health conditions.
To date, only five out of 23 patients have been reported to have received delayed surgical treatment [4,8-11]. Four of these patients presented late to the hospital, while one patient’s surgery was postponed due to abnormal neurological findings [11]. Our patient was unable to undergo emergency surgery because of SAH and hemopneumothorax accompanied by a flail chest. Enucleation was deemed necessary as the eyeball was non-viable, and the damage to the optic nerve was assessed to be irreversible. Unlike the previous five cases where there was no detailed description of the condition of the severely injured eyeball during the delay in treatment, we opted to continue conservative management of both the affected orbit and the displaced eyeball. Our goal was to preserve as much of the remaining orbital contents as possible and to prevent infection. To mitigate the progression of traumatic optic neuropathy, we administered topical corticosteroid eye drops. Additionally, to minimize the risk of an infection, we applied an antibiotic eye ointment and performed repeated sterile saline irrigations.
An anophthalmic socket differs from a normal eye socket. Enucleation can cause a reduction in orbital volume, redistribution of fat, and retraction of the EOMs, potentially leading to PESS. Additionally, osteoclastic activity may cause a hydroxyapatite implant in a reconstructed orbit to shrink, resulting in further loss of orbital volume [6-8].
The above-described structural alterations lead to a rotational displacement of the orbital contents in a posterior and inferior direction. This displacement exacerbates the deepening of the upper eyelid sulcus, causes ptosis with a drooping upper eyelid, tilts the superior fornix backward, and results in a loosening of the lower eyelid with a shallower inferior fornix. As these hallmark features of PESS advance, the application of an ocular prosthesis becomes unfeasible due to the loss of supporting structures and backward tilting. These compounding issues ultimately aggravate PESS, leading to more severe orbito-ocular deformities [6-8].
We implemented a strategy of transient conformer placement, followed by delayed orbital floor reconstruction and ocular prosthesis replacement, to minimize deformities related to PESS. Our patient tolerated the procedure well, with full recovery of both general condition and aesthetic appearance, despite the presence of late enophthalmos exceeding 5 mm.
To the best of our knowledge, the details of delayed treatment and the clinical course of traumatic dislocation of the eye into the maxillary sinus have not been previously described. Therefore, we aimed to propose an algorithm for the delayed treatment of traumatic eyeball dislocation into the maxillary sinus, drawing on our clinical experience and a review of the literature (Fig. 5).
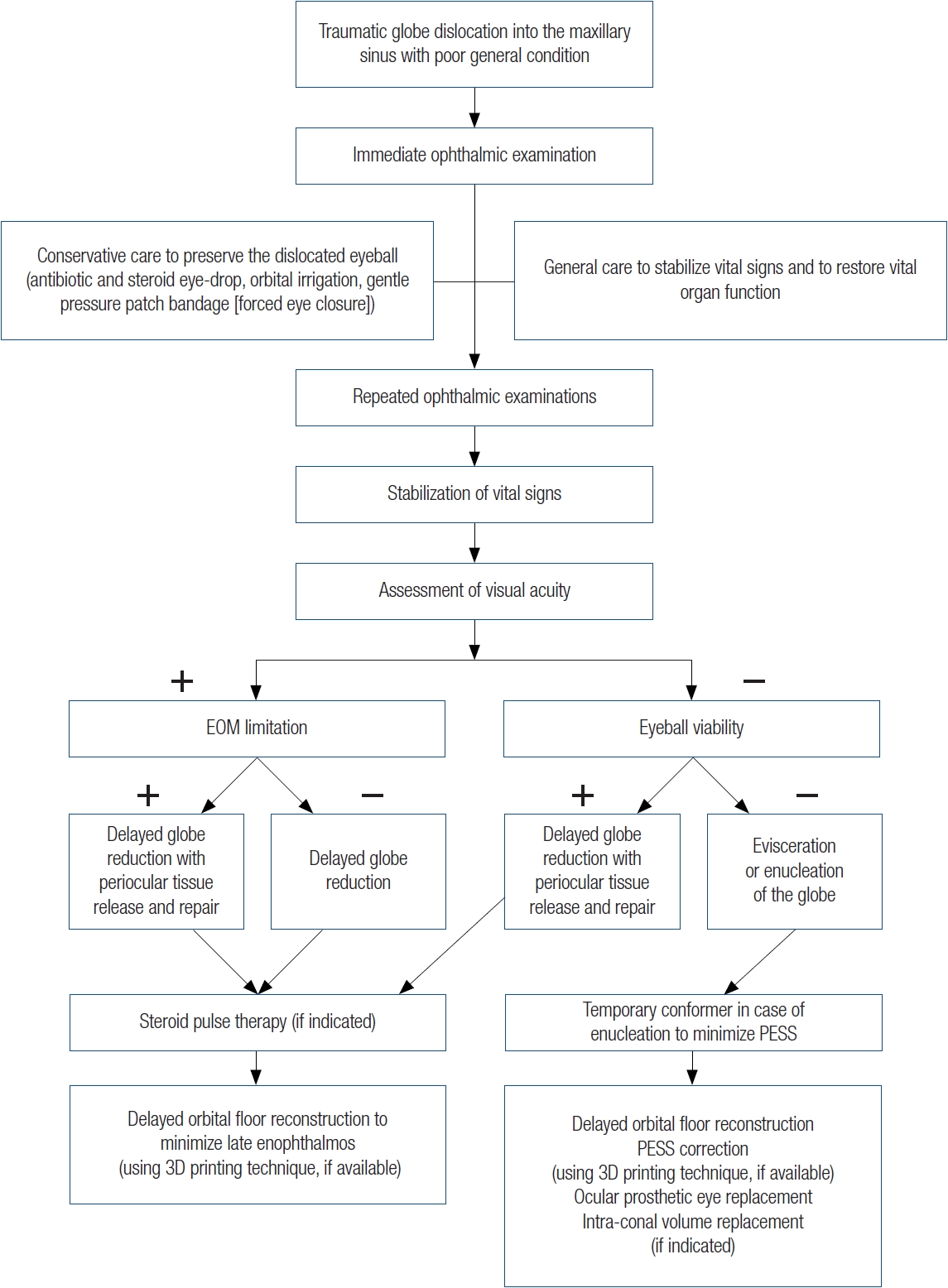
Delayed treatment algorithm for traumatic globe dislocation. EOM, extraocular muscles; 3D, three-dimensional; PESS, post-enucleation socket syndrome.
When treating a patient with traumatic dislocation of the eyeball into the maxillary sinus and an extensive orbital floor fracture, who also presents with poor general health, the initial step should be to stabilize the patient’s overall condition. Concurrently, an immediate ophthalmic examination is essential, along with conservative measures to preserve the displaced eyeball and orbit. Should visual acuity be present, it is advisable to perform eyeball reduction, with or without the release of periocular tissues, and repair. This procedure may be accompanied by steroid pulse therapy to mitigate traumatic optic neuropathy [3,4,28]. On the contrary, if vision loss is accompanied by a non-viable eyeball, evisceration or enucleation should be considered. Following enucleation, placement of a temporary conformer may be performed to minimize PESS [29,30]. Finally, delayed orbital floor reconstruction, followed by the placement of an ocular prosthesis, can be considered as a treatment option. To enhance symmetry and address aesthetic concerns, three-dimensional orbital reconstruction with a mirrored patient-specific implant may be utilized when available [31,32].
Depending on the patient’s clinical course, further surgical intervention may be necessary in cases of late enophthalmos or progressive PESS. A variety of surgical techniques can be tailored to address specific symptoms. For worsening enophthalmos, for example, intraconal volume replacement may be indicated [6,28]. Adjustments to the size and positioning of an ocular prosthesis can be made to correct for any deepening of the upper eyelid sulcus. Additionally, a non-absorbable ocular implant of the appropriate size may prove beneficial [6,28]. In the case we report, PESS was ultimately unavoidable. However, the patient was satisfied with the surgical outcome and managed to wear an ocular prosthesis without further progression of PESS or enophthalmos over a 2-year follow-up period.
For the development of an optimal standardized treatment algorithm, it is necessary to increase the number of patients. Our study has a clear limitation in that it includes only one case, and the treatment algorithm provided is based on a single clinical experience supplemented by a review of the literature. However, considering the rarity of delayed treatment for traumatic dislocation of the eyeball into the maxillary sinus due to poor general condition, our report could serve as a valuable treatment option or as a clinical reference.
Notes
Conflict of interest
No potential conflict of interest relevant to this article was reported.
Funding
None.
Ethical approval
The case report was approved by the Institutional Review Board of the Konyang University Hospital (No. 2020-12-023).
Patient consent
Written informed consent was obtained from the patient to publish and use her images.
Author contributions
Conceptualization: Soo Yeon Lim. Data curation: Keun Hyung Kim, Ga Hyun Lee. Formal analysis: In Chang Koh. Project administration: Hoon Kim. Writing - original draft: Keun Hyung Kim. Writing - review & editing: Hoon Kim, Keun Hyung Kim, In Chang Koh. Investigation: Keun Hyung Kim. Resources: Hoon Kim, In Chang Koh. Supervision: Hoon Kim, Soo Yeon Lim. Validation: Hoon Kim, In Chang Koh, Soo Yeon Lim.
Abbreviations
CT
computed tomography
EOM
extraocular muscles
ICU
intensive care unit
PESS
post-enucleation socket syndrome
SAH
subarachnoid hemorrhage