 |
 |
- Search
| Arch Craniofac Surg > Volume 25(1); 2024 > Article |
|
Abstract
Notes
Ethical approval
The case report was approved by the Institutional Review Board of the Konyang University Hospital (No. 2020-12-023).
Patient consent
Written informed consent was obtained from the patient to publish and use her images.
Author contributions
Conceptualization: Soo Yeon Lim. Data curation: Keun Hyung Kim, Ga Hyun Lee. Formal analysis: In Chang Koh. Project administration: Hoon Kim. Writing - original draft: Keun Hyung Kim. Writing - review & editing: Hoon Kim, Keun Hyung Kim, In Chang Koh. Investigation: Keun Hyung Kim. Resources: Hoon Kim, In Chang Koh. Supervision: Hoon Kim, Soo Yeon Lim. Validation: Hoon Kim, In Chang Koh, Soo Yeon Lim.
Fig. 1.
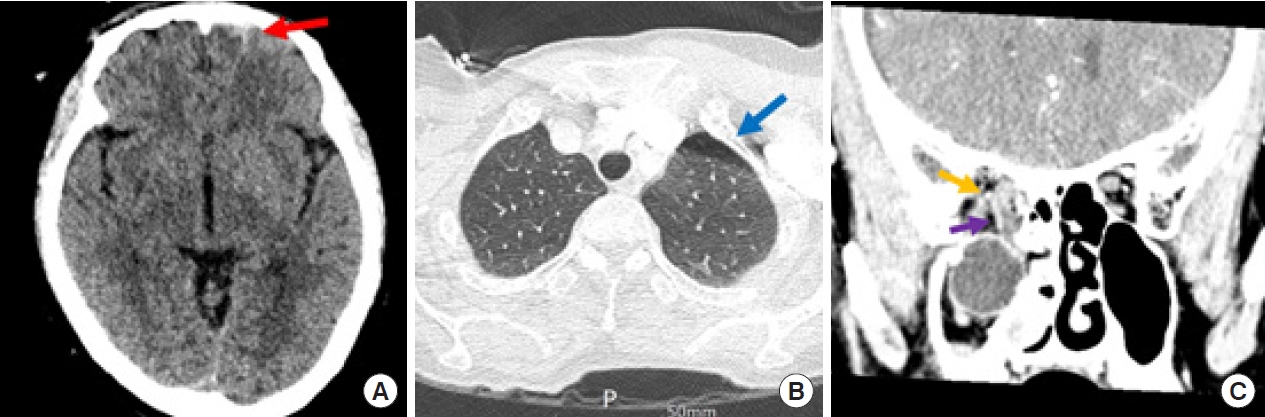
Fig. 2.

Fig. 3.
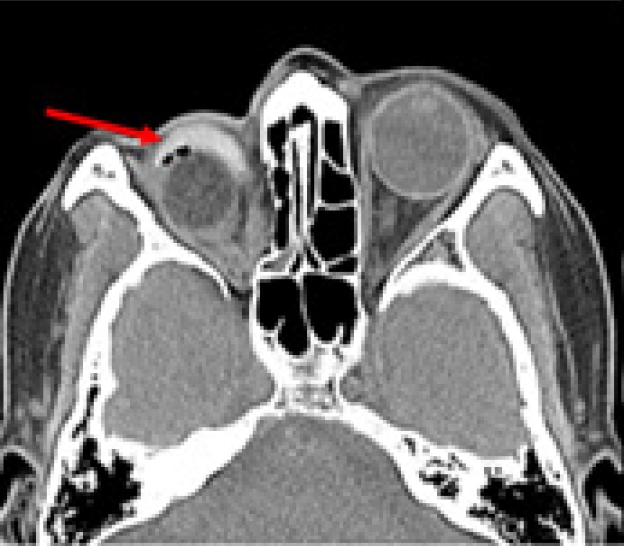
Fig. 4.

Fig. 5.
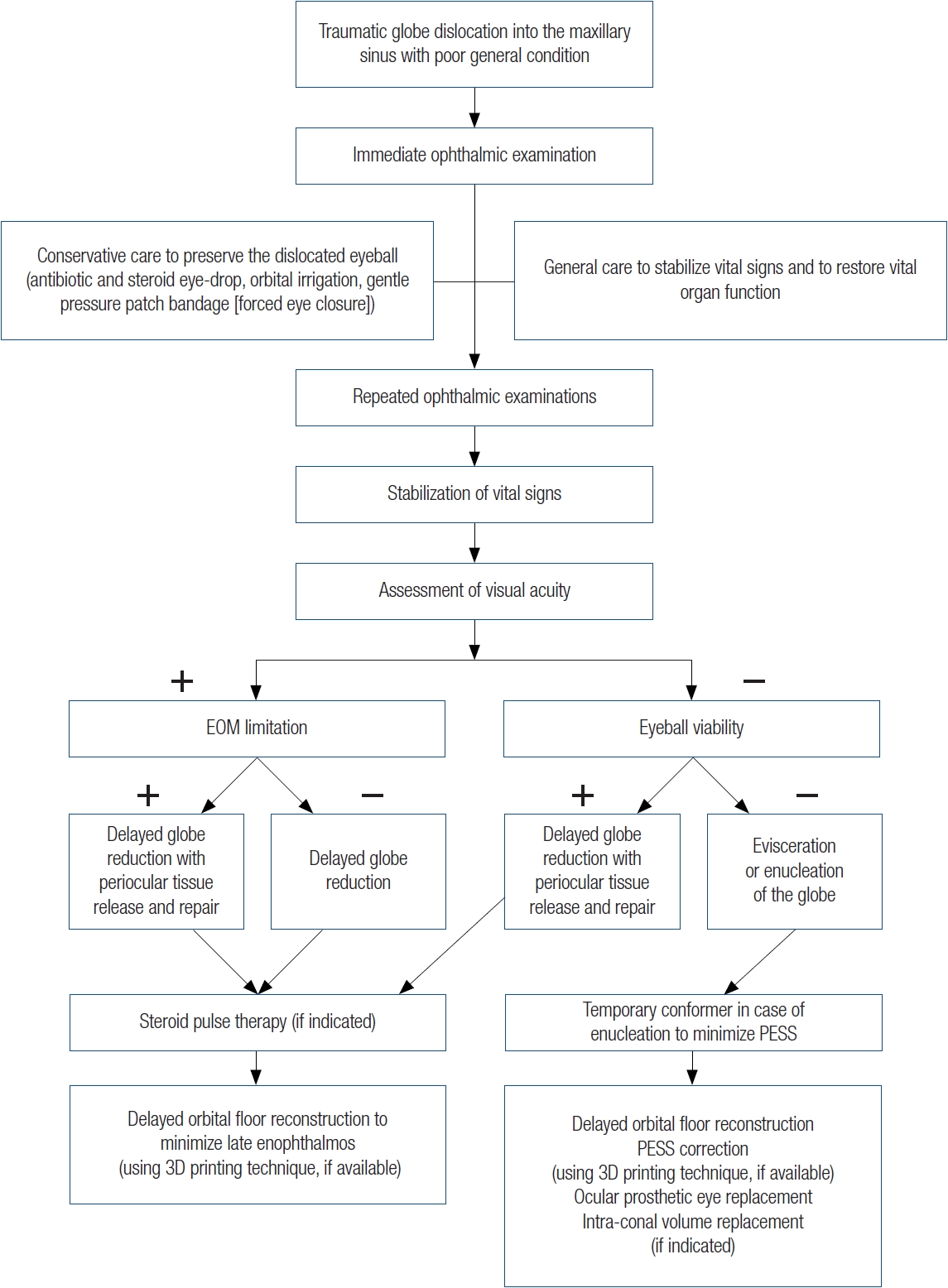
Table 1.
| Author | Timing of surgery relative to the emergency | Cause of delayed surgery | Injury type | Visual acuity | Globe repositioning | Orbital reconstruction | Enophthalmos (>2 mm) |
|---|---|---|---|---|---|---|---|
| Emery et al. [12] | NA | - | NA | NA | Direct traction | NA | NA |
| Immediate | - | NA | NA | Direct traction | NA | NA | |
| Stasior et al. [13] | NA | - | Fire hose injury | Recovery 20/60 | Maxillary antrostomy | No | Yes |
| Berkowitz et al. [14] | PTD 1 | - | Fist injury | Recovery 20/20 | Maxillary antrostomy | Silicone implant | No |
| Smit et al. [8] | 5 yr post-trauma | Late arrival at hospital | Windshield accident | No | NA | Teflon plate | Yes |
| Ziccardi et al. [15] | Immediate | - | Road traffic accident | Recovery 20/40 | Direct traction | Autogenous bone graft | Yes |
| Pelton et al. [16] | Immediate | - | Motor vehicle accident | NA | Maxillary antrostomy | NA | NA |
| Tung et al. [17] | Immediate | - | Motor vehicle accident | No | Direct traction | Autogenous bone graft | Yes |
| Saleh and leatherbarrow [9] | 2 mo post-trauma | Late arrival at hospital | Blunt trauma | No | Enucleation | Porous polyethylene | NA |
| Kim and Baek [18] | Immediate | - | Motor vehicle accident | No | Direct traction | Porous polyethylene | NA |
| Muller-Richter et al. [19] | Immediate | - | Farming machinery | Recovery 20/20 | Maxillary antrostomy | Balloon catheter | NA |
| Abrishami et al. [10] | PTD 7 | Late arrival at hospital | Car accident | No | Direct traction | Porous polyethylene | NA |
| Kreiner et al. [20] | Immediate | - | Collapsing wall | No | Direct traction | Silicone implant | Yes |
| Ramstead et al. [21] | Immediate | - | Bull fight | Recovery 20/200 | NA | Titanium mesh | NA |
| Zhang-Nunes et al. [22] | Immediate | - | Bike handlebar | Recovery 20/25 | NA | Silicone implant | NA |
| Xu et al. [23] | Immediate | - | Road traffic accident | Light perception | Direct traction | Titanium mesh | NA |
| Haggerty and Roman [24] | Immediate | - | Motor vehicle accident | Light perception | Maxillary antrostomy | Polytetrafluoroethylene | Yes |
| Amaral and Nery [4] | PTD 4 | Late arrival at hospital | Gym weight | Recovery 20/50 | Maxillary antrostomy | Titanium mesh | NA |
| Lim et al. [25] | NA | - | Metal edge | No | Direct traction | Autogenous bone graft | NA |
| Noman and Shindy [26] | Immediate | - | Blunt trauma (wooden object) | Recovery 20/40 | Maxillary antrostomy | Titanium mesh | NA |
| Bastos et al. [3] | Immediate | - | Fist injury | No | Maxillary antrostomy | Titanium mesh | Yes |
| Wang et al. [27] | NA | - | Penetrating tree branch | No | NA | Titanium mesh | NA |
| Alam et al. [11] | PTD 3 | Abnormality in a neurologic examination | Falling door | Finger count 1 m | Direct traction | Titanium mesh | No |
REFERENCES
- TOOLS
-
METRICS

-
- 0 Crossref
- Scopus
- 1,155 View
- 34 Download
- Related articles in ACFS
-
Intraosseous vascular malformation of the skull: a case report and literature review ;0()
Basal cell adenoma of parotid gland: two case reports and literature review2023 August;24(4)






