Distribution of maternal risk factors for orofacial cleft in infants in Indonesia: a multicenter prospective study
Article information
Abstract
Background
The pathogenesis of orofacial cleft (OFC) is multifactorial, involving both genetic and non-genetic factors, the latter of which play a key role in the development of these anomalies. This paper addresses the incidence of OFC in Indonesia, with a focus on identifying and examining the distribution of contributory factors, including parental medical history, pregnancy history, and environmental influences.
Methods
The study was conducted through the collection of primary data. An interdisciplinary research team from Indonesia administered a standardized questionnaire to parents who had children with OFC and who had provided informed consent. The case group comprised 133 children born with cleft lip and/or palate, and the control was 133 noncleft children born full-term. The risk factors associated with OFC anomalies were analyzed using the chi-square test and logistic regression. All statistical analyses were performed using SPSS version 25. A p-value of 0.05 or less was considered to indicate statistical significance.
Results
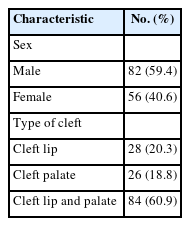
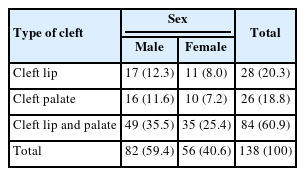
The study comprised 138 children, of whom 82 were boys (59.4%) and 56 were girls (40.6%). Among them, 45 patients (32.6%) presented with both cleft lip and cleft palate, 25 individuals (18.1%) had a cleft palate only, and 28 patients (20.3%) had a cleft lip only. OFC was found to be significantly associated with a maternal family history of congenital birth defects (p< 0.05), complications during the first trimester (p< 0.05), consumption of local fish (p< 0.05), caffeine intake (p< 0.05), prolonged medication use (p< 0.05), immunization history (p< 0.05), passive smoking (p< 0.05), and X-ray exposure during pregnancy (p< 0.05).
Conclusion
The findings indicate close relationships between the incidence of OFC and maternal medical history, prenatal factors, and environmental influences.
INTRODUCTION
Orofacial cleft (OFC) is a congenital disorder that impacts the mouth and associated structures [1]. These congenital defects can include structural, functional, or metabolic irregularities and currently pose a public health challenge [2]. The global incidence of OFC ranges from approximately 1.39 to 2 cases per 1,000 live births annually [1,3,4]. The frequency of this condition varies across ethnic groups, with the highest rates observed in Asia and the lowest in Afro-Caribbean populations [4].
OFC arises from developmental disruptions during pregnancy [5]. Maternal exposure to certain risk factors during pregnancy has been recognized as a non-genetic contributor to OFC [3]. The etiology of this condition is multifactorial and highly complex, but it is believed to stem from the interaction between genetic predispositions and a variety of environmental and dietary factors [1,3,6]. If risk factors are known, prophylactic and preventive measures can be implemented to diminish their impact [7]. The present research, therefore, focused on identifying and examining the distribution of risk factors for cleft lip and/or palate (CL/P), particularly those linked to maternal health history and environmental exposures during pregnancy.
METHODS
This study is a prospective, descriptive quantitative research investigation that received approval from the Research Ethics Commission of Padjadjaran University Bandung (approval number 882/UN6.Kep/EC/2023, dated July 10, 2023). Data were collected from various regions in Indonesia between July and September 2023. The primary variables of interest in this study related to the mothers of patients with CL/P, with a focus on risk factors that may contribute to the development of these conditions, specifically in relation to maternal health history and environmental exposures during pregnancy.
The study population, located in the western and eastern regions of Indonesia, was selected based on specific characteristics defined by the researchers to facilitate analysis and drawing of conclusions. The primary data consisted of outcomes from structured questionnaires administered through face-to-face interviews with mothers who had given birth to infants with CL/P and who were presenting for surgery in the respective provinces of the study, having provided informed consent. The case-control data were on children born at term without cleft lip and/or cleft palate.
Data collected from three provinces in Indonesia–DKI Jakarta, West Java, and South Sulawesi–were presented as numbers (percentages). For statistical analysis, this study employed the chi-square test and logistic regression. All statistical analyses were conducted using SPSS version 25 (IBM Corp.). A p-value of less than 0.05 was considered to indicate statistical significance.
RESULTS
This study included 138 mothers and children. Of the children, 59.4% were male and 40.6% female. The most frequently observed form of cleft was combined cleft lip and palate, accounting for 60.9% of cases, while isolated cleft palate was the least common, representing just 18.8%. When examining the distribution of cleft types by sex, the greatest proportion of patients were male children with cleft lip and palate, constituting 35.5% of cases. Detailed frequencies and percentages of these variables are presented in Tables 1 and 2.
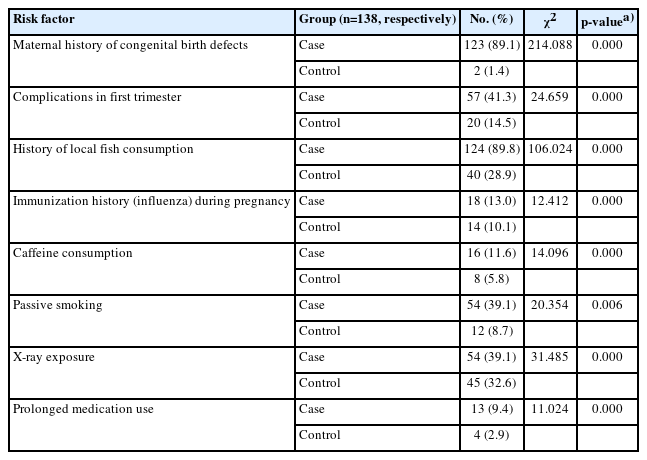
The distribution of risk factors associated with CL/P, in relation to maternal health history and environmental exposures during pregnancy, revealed several significant findings. A history of congenital birth defects was present for 10.9% of the mothers, while maternal complications in the first trimester were reported in 55% of cases. Fish consumption, primarily from local sources, was reported by 89.9%. Not being immunized during pregnancy was noted in 13% of cases, caffeine consumption in 11.6%, and long-term medication use in 9.4%. Passive smoking was identified in 38% of cases, and X-ray exposure during pregnancy 39.1%. These factors significantly influenced the incidence of OFC in newborns (p<0.05), as detailed in Table 3.
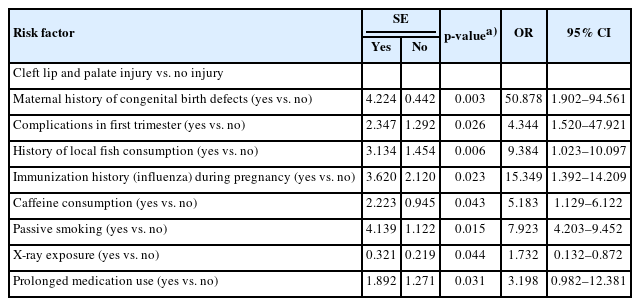
The chi-square test and logistic regression analyses were conducted to assess the relationship between the independent and dependent variables. Significance values obtained exceeding the 0.05 threshold were excluded, as it can be concluded that the independent variable has no significant influence on the dependent variable with respect to the type of cleft and the factors previously described as detailed in Table 4. The effect of each risk factor is shown through regression test. In this study, there was a significant relationship between each risk factor and the cleft type variable studied.
DISCUSSION
This study examined maternal exposure to risk factors associated with OFC during pregnancy. Identifying such factors will enable the development of preventive measures to reduce or manage exposure among pregnant women, particularly in the first trimester. By avoiding risk factors and ensuring early diagnosis of potential clefts, it may be possible to lessen or prevent their occurrence. CL/P represents one of the most common forms of OFC worldwide [3]. In Indonesia, the absence of a dedicated database for patients with CL/P means that we were unable to determine the incidence rate in our country due to the inability to access all cases. The rate of CL/P may differ across nations, as indicated by some studies [8,9]. In our sample, the majority of cases were found in the eastern region of Indonesia, accounting for 55.8% of the total.
A maternal history of birth defects is considered a genetic risk factor. In a 2015 study conducted by Figueiredo et al. [10] across Africa, Southeast Asia, and Central America, a maternal family history of clefts, as well as the presence of clefts in other siblings, were strongly associated with an increased risk of CL/P. Extensive research has led to the identification of two confirmed susceptibility loci, IRF6 and 8q24, in addition to at least 20 other genes or genomic regions that have been discovered or validated through genome-wide association studies [11]. However, the evidence is now mixed. It is plausible that genes exerting a minor genetic effect may also contribute to the risk by interacting with other genes or environmental risk factors [12]. Genetic testing can be instrumental in evaluating the recurrence risk for parents and other family members [13].
Complications arising in the first trimester may elevate the risk of CL/P. Our study identified several issues occurring during the first trimester of pregnancy, including stress, red spotting, falls, and vomiting, with the last of these being the most frequent. The embryonic development of the palate occurs between the fourth and the 12th to 13th weeks of gestation [14]. During this time, the fundamental facial morphology is established through the fusion of five primary facial prominences: the frontonasal prominence at the midline, and the paired maxillary and mandibular prominences [15]. Disruptions in a single gene due to external factors during pregnancy can interfere with the migration or proliferation of neural crest cells. These cells are responsible for a wide range of craniofacial malformations, including cleft palate [12,14,16].
A history of consuming locally sourced fish was found to significantly influence the incidence of cleft lip and palate. Dioxins are among the primary contributors to the development of congenital craniofacial defects [17]. These compounds, a varied collection of organic chemicals derived from oxanthrene and fumarate, are imperceptible to the senses and are commonly present in plastic waste [18]. Dioxins exert their effects primarily by inducing inflammation, thereby impacting various metabolic processes, such as bone mineralization and embryonic development. Fish accumulate dioxins from their environment via contact with water and sediment, but their primary source of exposure is dietary [19].
Given the common nature of coffee consumption among pregnant women, even a slight increase in the risk of malformations warrants caution [20]. In a systematic review of studies on OFC and caffeine, high intake was associated with a slight elevation in risk [21]. While the exact mechanism by which coffee consumption increases the risk of oral cleft remains unclear, it is believed that the effect on homocysteine levels contributes to the heightened risk of CL/P [22,23]. Furthermore, it has been demonstrated that the combination of coffee consumption and exposure to tobacco smoke can lead to increased plasma homocysteine concentrations [24].
The present study revealed chronic medication use as a significant risk factor for the increased incidence of CL/P. Additionally, medication use has been found to be significantly associated with elevated OFC risk, alongside dietary, nutritional, and lifestyle factors [7]. Numerous epidemiological investigations have explored the relationship between OFC and the use of medications or multivitamins. Excessive intake of these substances during pregnancy is significantly correlated with an elevated risk of OFC [3,25,26]. Although our study’s results did not identify the specific medications used, the reported drug use was in response to complaints of nausea and vomiting during the first trimester. In 2018, Huybrechts et al. [27] investigated the use of receptor antagonist drugs and discovered a modestly increased risk for the occurrence of OFC.
A history of influenza vaccination during pregnancy was also shown to significantly influence the incidence rate of OFC. In the present study, we did not inquire specifically about the type of vaccine administered. Our results differ from certain previous studies. For instance, Kharbanda et al. in 2017 [28] examined the association between the administration of the influenza vaccine in the first trimester of pregnancy and the risk of birth defects, concluding that maternal exposure to the influenza vaccine during the first trimester was not linked to increased risk. Similarly, Kabir et al. in 2021 [29] found that mothers who completed the vaccination program during pregnancy had a lower incidence of children with OFC compared to mothers who did not receive the full course of vaccinations.
Exposure to chemicals was additionally found to be associated with increased risk of CL/P. Similarly, passive smoking has been identified as a risk factor, as demonstrated in the study by de Andrade et al. in 2023 [30]. Specifically, exposure to second-hand smoke during the first trimester is linked to a heightened risk of oral clefts in children. When inhaled, carbon dioxide dissociates in the mother’s body, enabling nicotine to exert a vasoconstrictive effect and reducing uterine blood flow to the placenta. Furthermore, carbon monoxide competes with oxygen for binding to hemoglobin, leading to reduced oxygen availability to the placenta and consequent hypoxia [24].
X-ray exposure during pregnancy as the last risk factor identified in our study. This finding aligns with the 2020 results presented by Regina Altoe et al. [31], who identified exposure to ionizing radiation as a contributing factor to cleft lip. Similarly, Rakotoarison et al. in 2012 [32] observed that high doses of ionizing radiation from former mining operations were associated with an increased prevalence of clefts in the Vakinankaratra region of Madagascar. However, these results warrant further investigation. Ionizing radiation inflicts damage on living organisms by causing stochastic harm to one or both strands of the DNA double helix, thereby disrupting cellular function [33].
In conclusion, the incidence of OFC was found to increase in association with maternal history of congenital birth defects, complications during the first trimester of pregnancy, local fish consumption, caffeine intake, prolonged drug use, exposure to chemicals, X-ray exposure, immunization practices, and passive smoking during pregnancy. The etiology of clefts is multifactorial. While the data remain small, it is conceivable that genes exerting a modest genetic influence may also contribute to risk via interactions with other genetic elements or environmental risk factors.
Notes
Conflict of interest
No potential conflict of interest relevant to this article was reported.
Funding
None.
Ethical approval
The study was approved by the Institutional Review Board of Padjadjaran University Bandung (approval number 882/UN6. Kep/EC/2023) and performed in accordance with the principles of the Declaration of Helsinki. Written informed consent was obtained.
Author contributions
Conceptualization: Andi Tajrin, M. Ruslin, Muh. Irfan Rasul, Katharina Oginawati, Nurul Fahimah, Ikeu Tanziha, Annisa Dwi Damayanti, Utriweni Mukhaiyar, Asri Arumsari, Ida Ayu Astuti, Farah Asnely Putri, Shinta Silvia. Data curation: Andi Tajrin, Asri Arumsari. Formal analysis: Andi Tajrin, Husni Mubarak. Methodology: Andi Tajrin, M. Ruslin, Muh. Irfan Rasul, Katharina Oginawati, Nurul Fahimah, Ikeu Tanziha, Annisa Dwi Damayanti, Utriweni Mukhaiyar, Asri Arumsari, Ida Ayu Astuti, Farah Asnely Putri, Shinta Silvia. Project administration: Andi Tajrin, Husni Mubarak. Visualization: Andi Tajrin. Writing - original draft: Andi Tajrin, M. Ruslin, Muh. Irfan Rasul, Husni Mubarak, Nurul Fahimah, Nurwahida, Hadira, Katharina Oginawati, Nurul Fahimah, Ikeu Tanziha, Annisa Dwi Damayanti, Utriweni Mukhaiyar, Asri Arumsari, Ida Ayu Astuti, Farah Asnely Putri, Shinta Silvia. Writing - review & editing: Andi Tajrin. Investigation: Andi Tajrin, Husni Mubarak. Supervision: Andi Tajrin.
Abbreviations
CL/P
cleft lip and/or palate
OFC
orofacial cleft