Abbreviations:
isolated unilateral temporalis muscle hypertrophy
;
magnetic resonance imaging
;
nonsteroidal anti-inflammatory drug
;
INTRODUCTION
Isolated unilateral temporalis muscle hypertrophy (IUTMH) is a rare condition that presents as localized swelling in the temporal region [
1]. Its etiology remains unclear. Though it can be a compensatory response or result from stress-induced temporalis muscle hypertrophy, careful differential diagnosis should be performed to rule out other conditions like inflammation or infection, neoplasms, myopathy, and genetic issues [
1,
2]. The diagnosis of IUTMH relies on meticulous clinical observations, radiological imaging such as computed tomography (CT) and magnetic resonance imaging (MRI), and temporalis muscle biopsy when needed. Treatment involves mitigating related risk factors, providing supportive care, potentially performing temporalis muscle reduction surgery, or administering intramuscular botulinum toxin A (Btx A) injections [
2,
3]. Wilson and Brown [
4] first documented IUTMH in 1990. IUTMH is so rare that only 14 cases have been reported in the English-language literature over the past three decades. This study seeks to present an effectively diagnosed and treated case of IUTMH, accompanied by a literature review.
CASE REPORT
A 39 year-old woman sought medical assistance at our clinic with a painless swelling in her left temporal area that had been present for a month. Aside from a decade-long treatment for hypothyroidism, she had no significant medical history. The patient had not experienced head trauma, notable dietary changes, bruxism, headaches, or undergone any surgery recently. However, she had received Btx A injections in both masseter muscles for cosmetic reasons a year ago, and had been under severe personal stress for 3 to 4 months.
Upon physical examination, the patient presented with a soft, diffuse swelling in her left temporal area, devoid of tenderness. The swelling hardened and protruded when she clenched her teeth. According to the patient the swelling fluctuated in size, being larger in the morning and becoming smaller as the day progressed. No signs indicative of inflammatory changes, such as pain, fever, warmth, tenderness, or erythema, were observed. Furthermore, oral, dental, and temporomandibular joint examinations did not reveal any notable findings.
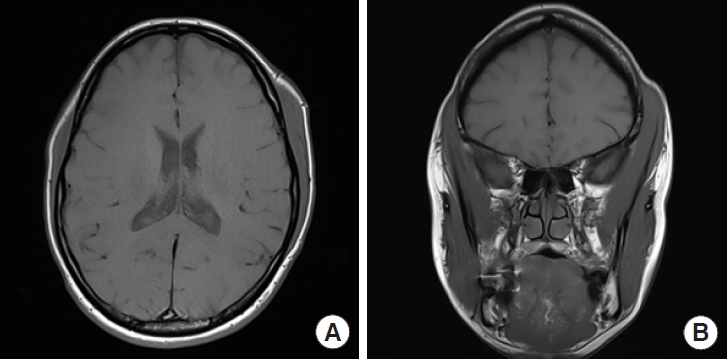
Contrast-enhanced MRI revealed an asymmetrically homogenous hypertrophy of the left temporalis muscle, excluding the masseter muscle. No lymph node enlargement was detected, and no intra- or extra-cranial abnormalities were present (
Fig. 1). The combination of clinical examination and radiologic findings led to the diagnosis of IUTMH.
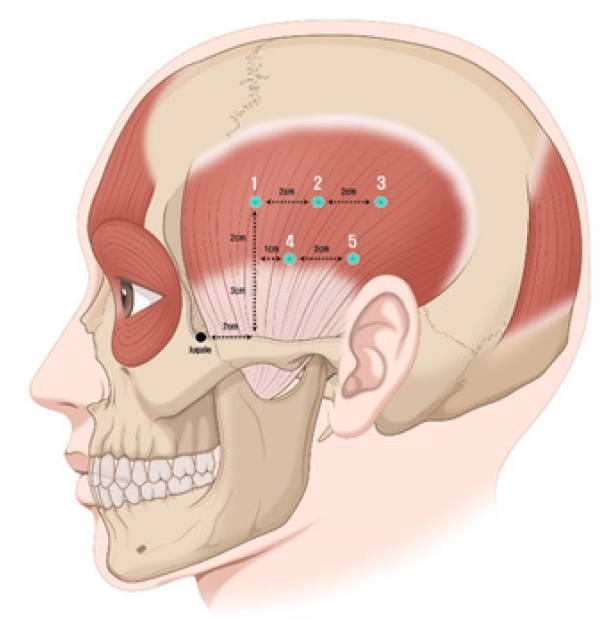
Supportive treatment involving stress reduction, avoidance of foods that could irritate the masseter muscle, and discouragement of teeth clenching was provided for the first month but yielded minimal effectiveness. Consequently, 25 units of Btx A (Botulax; Hugel Inc.) were administered at five distinct points into the left temporalis major, with careful consideration of the course of deep temporal nerve (
Fig. 2) [
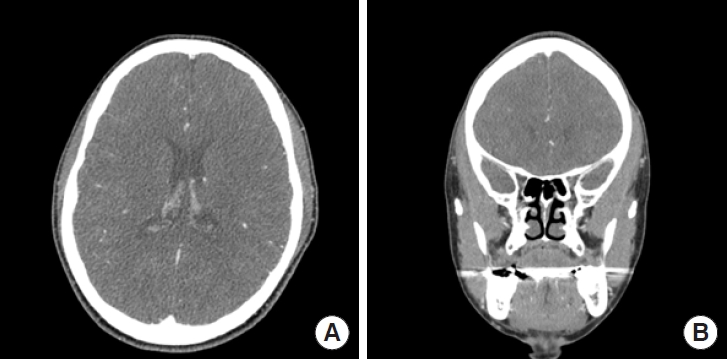
5]. The asymmetrical hypertrophy in both temporal regions significantly improved to the naked eye, restoring symmetry to the temporal areas. The patient did not experience functional issues such as masticatory movement disorders during mouth opening or eating. While she reported some residual swelling in the mornings, it had noticeably lessened. Nine months posttreatment, no recurrence or other significant findings were noted during observation. There were no subjective symptoms of the patient. Furthermore, contrastenhanced CT showed highly improved outcome at 9-month follow-up (
Fig. 3). The patient was highly satisfied with the treatment outcome and preferred to monitor progress without undergoing additional laboratory or histological examinations.
LITERATURE REVIEW
We conducted a literature review by analyzing cases of IUTMH in articles available up to the year 2023, sourced from PubMed and Google Scholar. A total of 15 patient cases, including our own, from 14 different articles were scrutinized. We collated data encompassing age, sex, race, symptoms, location of swelling, onset, diagnosis, suspected cause, treatment, outcome, and follow-up period.
The 15 cases, including the case presented herein, were compared (
Table 1) [
1-
13]. The cohort comprised six males and nine females. Among them, eight experienced swelling on the right side of the temporal region and seven on the left. Swelling was more prevalent among female participants, with no significant difference observed between the left and right temporal regions. The average age was 31.5 years, ranging from 7 to 65 years, and only four patients were minors. At the time of the hospital visit, 11 patients reported painless swelling, four reported painful swelling, and two had a history of recurring headaches. The average duration from the onset of temporal swelling to the hospital visit was 12.7 months, with a range from 2 weeks to 8 years. All 15 cases underwent imaging studies for diagnosis, with nine of them also undergoing histological examinations. Regarding potential causes, two cases exhibited distinctive masticatory habits such as bruxism, two cases had experienced psychogenic issues due to stressful conditions according to their medical histories, and one case presented both masticatory habits and psychogenic problems.
Various treatment methods were employed for IUTMH. Patients with minor cosmetic concerns were diagnosed through imaging or histological tests, and their symptoms, such as headaches, were managed with analgesic medications, stress reduction measures, or supportive treatments such as wearing a maxillary splint [
1,
3,
4,
7,
9,
10,
13]. According to Rokadiya and Malden [
9], improvements in headaches and muscle hypertrophy were observed following the application of amitriptyline medications and Michigan splints. Other patients received symptomatic treatment using oral medications, with some reporting that the size of the IUTMH remained unchanged [
10,
13].
Two cases underwent treatment through partial temporalis muscle reduction surgery [
6,
8]. In one of these cases, where IUTMH recurred, the patient was successfully treated with a combination of muscle reduction surgery and Btx A injections [
8].
A significant number of cases were managed with intramuscular injections of Btx A. In total, six cases were treated with Btx A. In the study by Isaac [
5], the report of Prantl et al. [
8], and in our case, an improvement in the muscle contour of the temporal area was observed during the follow-up at 2 months, 6 months, and 9 months after Btx A injection, respectively. Katsetos et al. [
12] also noted an improvement after the treatment.
DISCUSSION
The phenomenon of masticatory muscle hypertrophy, involving the masseter, temporalis, and pterygoid muscles, was first brought to light by Legg [
14] in 1880, with a steady stream of cases reported thereafter. Most of these cases exhibited bilateral hypertrophy, with either both the masseter and temporalis muscles affected, or only one of them enlarged. Of these, IUTMH is extraordinarily rare [
1,
3,
13]. To our knowledge, this represents the 15th documented case of IUTMH in the international literature.
Masticatory muscle hypertrophy can be categorized into reactive and non-reactive types, and it is essential to differentiate between the two. Non-reactive enlargement, the more prevalent form of masticatory muscle hypertrophy, can be attributed to causes such as myopathy, idiopathic conditions, genetic issues, neoplasms, and origins of inflammatory or infectious nature. Reactive hypertrophy, on the other hand, stems from a gradual increase in masticatory muscle workload rather than a sudden surge. This category encompasses local bone or dental issues and parafunctional jaw habits [
1,
3,
15]. IUTMH falls under the category of reactive masticatory muscle hypertrophy and is characterized by benign enlargement of the temporalis muscle on one side, which may be either painful or painless. The precise cause of IUTMH remains unknown. Potential triggers include bruxism, malocclusion, temporomandibular joint disease, and trauma. In most instances, hypertrophy is prompted by psychogenic factors such as stress or anxiety, or compensatory responses [
1,
2]. In the case of our patient, no instances of bruxism, surgery, trauma, or temporomandibular joint disease were noted. However, it was discovered that the patient had encountered a significant amount of stress, which could have induced an enlargement of the temporalis muscle. It is also possible that reactive hypertrophy had been triggered by the injection of Btx A she had received in both masseter muscles a year ago [
16]. Mierzwa et al. [
16] reported a compensatory increase in stiffness of the temporalis muscles in patients who were treated with Btx A injection for bilateral masseter muscle hypertrophy. However. no significant difference between both temporalis muscles was seen. In the case presented here only unilateral temporalis muscle hypertrophy was seen. Furthermore, there is a considerable interval between the patientâs Btx A injections to the masseter and the appearance of the unilateral IUTMH. It can be suggested that the previously injected Btx A was already washed out. For these reasons, it is difficult to see this case as a secondary temporalis muscle hypertrophy due to former Btx A injection.
A diagnosis can be established based on clinical features and imaging studies. Homogeneous enlargement of the temporalis muscles can be detected via CT, MRI, or ultrasonography. Additionally, a temporalis muscle biopsy can aid in diagnosing IUTMH by distinguishing it from inflammatory diseases such as myopathy and fasciitis. Histochemical analysis typically reveals hypertrophy and a predominance of type 1 fibers, while inflammatory markers tested using antibodies for CD3, CD4, CD8, and CD20 yield negative results. Nevertheless, in some instances, a muscle biopsy may not be performed, and treatment is provided based solely on symptoms [
1,
2,
10,
12].
There are diverse treatment options for IUTMH. Symptoms such as headaches can be managed using analgesics such as acetaminophen, amitriptyline, or nonsteroidal anti-inflammatory drugs, and in certain instances, supportive treatment involving maxillary splints is employed [
3,
9,
10]. Btx A injections may be administered to patients who prefer to avoid invasive diagnostic and therapeutic procedures [
5,
11,
12]. In some cases, temporalis muscle reduction surgery is conducted [
6,
8]. However, surgery is typically reserved for patients with suspicious histological findings or a heightened fear of cancer. Furthermore, surgery may not fully eradicate underlying dysfunctions, which could potentially recur [
4].
Conversely, intramuscular Btx A injections offer several benefits. For instance, this treatment method is much simpler and less invasive compared to surgery. It also carries a lower risk of surgical complications such as trismus, fibrosis, and reduced range of motion. Btx A works by inhibiting the release of the neurotransmitter acetylcholine at the cholinergic nerve endings of the peripheral nervous system. This process induces selective muscle paralysis, leading to muscle atrophy and an improvement in associated symptoms such as headaches. However, a limitation is that the effects of Btx A therapy tend to fade after about 6 months, which could potentially lead to the recurrence of hypertrophy and necessitate periodic injections. In our case, there was no recurrence until 9-month follow-up after treatment. Given that this treatment can be administered in an outpatient clinic setting, and the cost of intramuscular Btx A injections is generally lower than surgical treatment, this represents a highly effective treatment option [
3,
5,
11,
17,
18].
Unfortunately, a temporalis muscle biopsy was not performed in the case described herein. Had such a biopsy been carried out, there is a small chance other differential diagnoses could have been detected. However, given that this patient had a clear clinical and radiological presentation and expressed a desire to avoid further laboratory and histological examinations, we elected to administer Btx A treatment and conduct subsequent outpatient follow-up examinations including radiologic imaging study.
In summary, IUTMH is an uncommon cause of temporal swelling. Treatment via intramuscular Btx A injection can effectively address IUTMH in a minimally invasive manner. Given its capacity to reduce the volume of temporalis hypertrophy without the complications associated with surgery and restore facial contour, it can be regarded as the treatment of choice.