|
 |
- Search
| Arch Craniofac Surg > Volume 25(3); 2024 > Article |
|
Abstract
A 76-year-old woman, initially thought to have a simple abscess on her right upper eyelid, presented to our department of plastic and reconstructive surgery. Enhanced three-dimensional facial computed tomography (CT) revealed an abscess on the right upper lid, with a pyomucocele present in the right frontal sinus, accompanied by bone erosion in the superior wall of the right orbit. Based on the results of the CT scan, we diagnosed an atypical Pott’s puffy tumor (PPT) with an abscess on the upper lid originating from the frontal sinusitis. First, surgical incision and drainage were performed in our department, and a percutaneous vacuum drain was placed. To provide a more definitive treatment, endoscopic sinus surgery (ESS) was subsequently performed by otorhinolaryngologists. The patient was discharged without any complications 5 days after ESS. At a 1-year follow-up, no recurrence or notable neurological symptoms were observed. In the case we observed, the patient presented with an upper eyelid abscess and cellulitis, indicating possible orbital involvement. For such patients, a CT scan is necessary. Given the possibility of PPT, it is critical to perform a comprehensive differential diagnosis rather than defaulting to a straightforward approach involving abscess treatment.
Pott’s puffy tumor (PPT), first described by the British neurosurgeon Percival Pott in 1775, is characterized by a subperiosteal abscess of the frontal bone with concurrent osteomyelitis, typically resulting from frontal sinusitis [1]. It often manifests as localized swelling and tenderness in the frontal region. However, additional symptoms such as headache, periorbital edema, purulent rhinorrhea, fever, and vomiting may also be present [2,3]. The presence of these symptoms warrants consideration of other intracranial complications, including epidural abscess, subdural empyema, or brain abscess, which require prompt diagnostic evaluation and treatment [2,4]. PPT is exceedingly rare, both in South Korea and internationally, especially in the era of widespread antibiotic use [5]. In this report, we describe an atypical presentation of PPT with a unilateral upper lid abscess and provide a literature review on the topic.
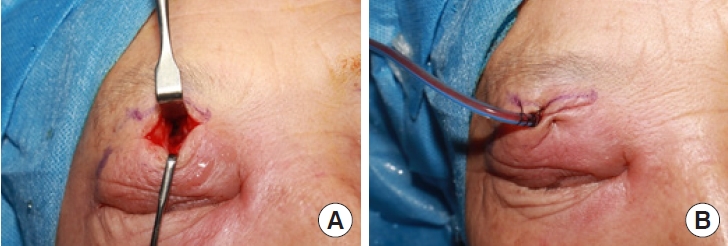
A 76-year-old woman presented to our clinic with a history of right upper eyelid swelling that had developed 2 weeks prior. She was referred from the department of ophthalmology at another hospital for further evaluation and management. The patient denied any trauma or systemic infections, and she had no history of cosmetic procedures. On physical examination, she exhibited difficulty opening her right eye due to swelling. There was no external wound or cutaneous opening; however, the area was tender upon palpation (Fig. 1). She was immediately admitted, and administration of antibiotics was initiated. Enhanced facial computed tomography (CT) showed a 2.5 cm subperiosteal abscess on the right superior orbital rim, extending from the frontal sinus, with accompanying bone erosion in the superior wall of the right orbit (Fig. 2). Based on the CT findings, we diagnosed an atypical type of PPT with a unilateral upper lid abscess.
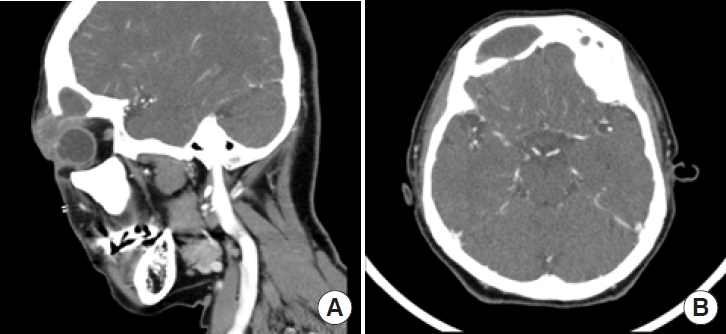
An incision was made over the abscess located beneath the orbicularis oculi muscle, extending inferiorly along the superior orbital rim to access the right frontal sinus. Soft tissue curettage was performed, followed by extensive irrigation using copious amounts of normal saline and betadine solution. A percutaneous vacuum drain was then inserted into the right frontal sinus through the supraorbital roof (Fig. 3).
Although symptoms such as swelling and redness improved after the surgery, a CT scan revealed signs of obstruction at the opening of the frontal sinus and an enlargement of the frontal sinus itself, along with evidence of mild erosion of the sinus wall. Additionally, nasal endoscopy revealed a deviation of the nasal septum to the right and a narrowed nasal passage. For definitive treatment, endoscopic sinus surgery (ESS) was performed by the otorhinolaryngological surgery team, and additional empirical intravenous antibiotics were administered to provide coverage against anaerobic bacteria. During the procedure, necrotic tissue was excised, and obstructions caused by bony structures were found in both frontal recesses. A right antrectomy, right middle turbinectomy, and bilateral frontal sinusotomy were carried out. A bacterial culture from the abscess showed no growth. Histopathological examination indicated chronic inflammation. The patient experienced no significant discomfort after the operation and was discharged without any complications 5 days after ESS. No recurrence or new lesions were observed at the 1-year follow-up (Fig. 4).
PPT, a complication of frontal sinusitis, is characterized by the formation of a subperiosteal abscess beneath the frontal bone, which may manifest as swelling in the forehead area. This condition has become uncommon due to the advent of antibiotics [6]. Nevertheless, without early diagnosis and appropriate antibiotic treatment, it can lead to serious complications such as meningitis, extradural abscess, subdural empyema, brain abscess, and cavernous sinus thrombosis. Among these intracranial complications, subdural empyema is the most common, followed by intracerebral abscess and meningitis. Understanding the unique anatomical structure and vascular supply of the frontal sinus is crucial for comprehending how infections spread and complications develop. The mucosa of the frontal sinus is connected to the valveless diploic veins of the frontal bone, which facilitates the hematogenous spread of bacteria or infectious thrombi, leading to intracranial complications [7]. PPT is more prevalent in children because the growth of the frontal sinus and the blood flow in the diploic system around the frontal bone peak between the ages of 7 and 20. This results in a higher incidence of frontal sinusitis during this developmental period [8].
Clinically, PPT can present with symptoms including swelling of the forehead, fever, headache, and tender swelling in the frontal region. Ophthalmic manifestations can include double vision, sensitivity to light, reduced visual acuity, and paralysis of the muscles that move the eye, known as oculomotor nerve palsy [9]. In some instances, a subcutaneous swelling in the frontal area may develop, which has been mistakenly diagnosed as anterior orbital cellulitis in reported cases. As the disease progresses, certain clinical symptoms, such as headache, may temporarily subside as the frontal region expands [10].
PPT is suspected as a complication of acute frontal sinusitis, informed by the patient’s medical history, presenting symptoms, and physical examination findings. These include headache, fever, and tender swelling in the forehead. However, symptoms may be mild in the early stages. Differential diagnosis should consider other conditions that present with forehead swelling, such as skin and soft tissue infections, infected hematomas, or skin tumors [11].
Radiological examinations, including contrast-enhanced CT, can aid in diagnosis; however, they may not clearly delineate the extent of the disease or specific radiological abnormalities in the early stages. Radionuclide bone scanning is helpful for diagnosing osteomyelitis and assessing its extent, while magnetic resonance imaging provides detailed information regarding the precise location and extent of the lesion [12].
The treatment of PPT requires appropriate antibiotic therapy, surgical debridement of necrotic bone tissue, and drainage of any abscesses. Initially, empirical treatment with broad-spectrum antibiotics effective against anaerobic bacteria is necessary until the results of culture and sensitivity tests are available. Once the causative bacteria are identified, targeted antibiotics should be administered intravenously to combat the specific strains. Common causative organisms include streptococci, staphylococci, Haemophilus influenzae, and various anaerobic bacteria, with the possibility of mixed infections involving both aerobic and anaerobic species. Early surgical intervention is critical for successful outcomes [1,6,8]. ESS may be utilized to address localized osteomyelitis or subperiosteal abscesses. In cases of more extensive lesions or intracranial complications, external approaches may be required, or collaboration with neurosurgery for a craniotomy may be necessary. Even with aggressive antibiotic therapy post-surgery, there is a risk of abscess recurrence, necessitating vigilant follow-up. Although PPT carries a high mortality rate of 5%–10% when sinusitis spreads to the intracranial space, the prognosis is generally favorable with timely and appropriate medical and surgical intervention. With such treatment, very few cases result in death or neurological sequelae [11,13].
In this case, preoperative nasal endoscopy and facial CT revealed a deviated nasal septum. The narrowed nasal passage resulting from the deviated septum could delay ventilation and drainage. Additionally, the decreased ciliary movement of the nasal mucosa, potentially due to nasal polyps, may have contributed to the development of frontal sinusitis [14,15]. Furthermore, frontal sinusitis can occur as a secondary infection due to obstruction in the frontal area caused by conditions such as sinusitis, allergic rhinitis, nasal polyps, tumors, or trauma [10].
The standard and preferred method for draining an abscess and debriding necrotic bone tissue is ESS. Although the literature does not explicitly state that this procedure should be performed in a stepwise fashion, in the case at hand, to prevent the abscess from spreading to the superior orbital and frontal sinuses, initial treatment focused on drainage. This was followed by collaborative surgery with the otolaryngology team for a more thorough intervention.
PPT, presenting as a complication of frontal sinusitis involving the intracranial or orbital regions, has become a rare condition since the introduction of antibiotics. Only a few cases have been reported in Korea. In this instance, the typical symptoms of PPT, which include headache, fever, and nasal discharge, were absent. An eyelid lesion was the sole observable symptom upon examination, representing an even rarer and atypical case.
In this case, there were no typical symptoms suggesting frontal sinusitis, and the condition could have been mistaken for a simple abscess. Therefore, an accurate differential diagnosis was crucial. Without it, treatment might have been ineffective, leading to recurrence or worsening of the condition and potentially resulting in severe complications. It is important to consider PPT and to perform imaging studies for the differential diagnosis when evaluating patients with an eyelid abscess.
Notes
Ethical approval
The report was approved by the Institutional Review Board of Hallym University Kangdong Sacred Heart Hospital (IRB No. 2023-08-004).
Fig. 1.
Preoperative photograph of a 76-year-old woman who had difficulty of opening her right upper eyelid due to an abscess, with no history of trauma or infection.
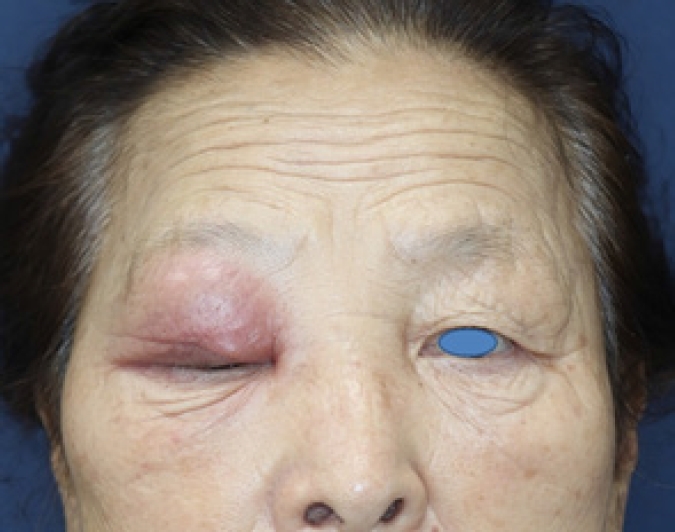
Fig. 2.
Preoperative enhanced facial computed tomography scan images of the patient. (A) The sagittal view showing a focal lowdensity area with peripheral rim enhancement, indicating a subperiosteal abscess spreading from the frontal sinus to the right upper eyelid through a bony defect in the orbital roof. (B) The axial view showing that the right frontal sinus displays asymmetrical enlargement, consistent with chronic sinusitis.
REFERENCES
2. Is M, Karatas A, Aytekin H, Dosoglu M, Gezen F. An 11-yearold girl with Pott’s puffy tumour. Int J Pediatr Otorhinolaryngol Extra 2007;2:215-7.

3. Haider HR, Mayatepek E, Schaper J, Vogel M. Pott’s puffy tumor: a forgotten differential diagnosis of frontal swelling of the forehead. J Pediatr Surg 2012;47:1919-21.


4. Huijssoon E, Woerdeman PA, van Diemen-Steenvoorde RA, Hanlo PW, Plotz FB. An 8-year-old boy with a Pott’s puffy tumor. Int J Pediatr Otorhinolaryngol 2003;67:1023-6.


5. Kim NE, Kim SS. A case of Pott’s puffy tumor from recurrent upper eyelid abscess. J Korean Ophthalmol Soc 2013;54:798-802.

6. Martinez-Diaz GJ, Hsia R. Pott’s puffy tumor after minor head trauma. Am J Emerg Med 2008;26:739.e1-3.


7. Bambakidis NC, Cohen AR. Intracranial complications of frontal sinusitis in children: Pott’s puffy tumor revisited. Pediatr Neurosurg 2001;35:82-9.



8. Lang EE, Curran AJ, Patil N, Walsh RM, Rawluk D, Walsh MA. Intracranial complications of acute frontal sinusitis. Clin Otolaryngol Allied Sci 2001;26:452-7.


9. Bannon PD, McCormack RF. Pott’s puffy tumor and epidural abscess arising from pansinusitis. J Emerg Med 2011;41:616-22.


10. Lamoreau KP, Fanciullo LM. Pott’s puffy tumour mimicking preseptal cellulitis. Clin Exp Optom 2008;91:400-2.


11. Verbon A, Husni RN, Gordon SM, Lavertu P, Keys TF. Pott’s puffy tumor due to Haemophilus influenzae: case report and review. Clin Infect Dis 1996;23:1305-7.

12. Goldberg AN, Oroszlan G, Anderson TD. Complications of frontal sinusitis and their management. Otolaryngol Clin North Am 2001;34:211-25.


13. Park J, Kim WS, Kim HK, Bae TH. Intracranial abscess from facial cellulitis. Arch Craniofac Surg 2019;20:332-5.




- TOOLS
-
METRICS

-
- 0 Crossref
- Scopus
- 922 View
- 32 Download
- Related articles in ACFS
-
Intraosseous vascular malformation of the skull: a case report and literature review ;0()